
Risk of Nutritional Deficiencies and Changes in Dietary Patterns after Bariatric Surgery
RehabilitationReceived 03 Mar 2025 Accepted 31 Mar 2025 Published online 01 Apr 2025
Focusing on Biology, Medicine and Engineering ISSN: 2995-8067 | Quick Google Scholar
Next Full Text
A Comprehensive Review of Federated Learning in Cancer Diagnosis and Prognosis Prediction


Received 03 Mar 2025 Accepted 31 Mar 2025 Published online 01 Apr 2025
Background: Nutrient deficiency and dietary restriction are common after bariatric surgery, regardless of weight loss. We aimed to evaluate the postoperative change in dietary patterns.
Methods: 113 patients who underwent bariatric surgery from 2018 to 2021 were followed up at baseline and three months after surgery. Anthropometric and biochemical data were collected retrospectively, and the diet was analyzed by a food frequency questionnaire (FFQ).
Results: Postoperative weight, body mass index (BMI), and % body fat decreased significantly (p < 0.001). Prealbumin (PA) and retinol-binding protein (RBP) levels decreased significantly at 3 months post-surgery (p < 0.001); however, vitamin D (VD), zinc, and albumin (ALB) levels increased (p < 0.05). Hemoglobin (HGB) in the Roux-en-Y gastric bypass (RYGB) group was lower than that in the sleeve gastrectomy with jejunal bypass (SGJB) and the sleeve gastrectomy (SG) group (p < 0.05). The intake of cereals, tubers, legumes, meat, poultry, and aquatic products decreased (p < 0.001), whereas the intake of vegetables (except for soybeans), fruit, eggs, milk and dairy products, and water increased (p < 0.05). The RYGB group had a higher intake of cereals, tubers, and legumes than that in the other groups (p < 0.05), although there was no association between the reduction of intake in these food groups and weight loss.
Conclusion: Bariatric surgery has a beneficial impact on weight loss and dietary patterns. Preoperative nutritional assessment and continuous follow-up are critical with bariatric surgery to prevent weight regain and malnutrition.
Currently, more than 2.2 billion people, representing 40% of the global population, are classified as overweight or obese []. Data from the China Chronic Disease and Nutrition Surveillance surveys (2015–2019) indicate that the prevalence rates of overweight and obesity in China are 34.3% and 16.4%, respectively, making China second only to the United States in obesity prevalence [,]. Bariatric surgery is recognized as an effective intervention for obesity, offering substantial weight reduction and mitigating obesity-related comorbidities, such as type 2 diabetes, cardiovascular diseases, hypertension, and certain cancers []. It has also been shown to delay the progression of chronic kidney disease []. Additionally, bariatric surgery reduces the risk of premature mortality by 30%–50% and enhances health-related quality of life [,]. Post-surgery, patients achieve excess weight loss (%EWL) of 31.6%, 60%, and 77% at three, six, and twelve months, respectively, with maximum weight loss typically occurring within two years. Long-term outcomes indicate that 50% EWL is maintained five years post-surgery [,].
Restrictive procedures, such as sleeve gastrectomy (SG), limit food intake by removing the larger, curved portion of the stomach, while malabsorptive procedures bypass sections of the intestine, significantly reducing nutrient absorption due to decreased contact between the intestinal epithelium and nutrients [,]. Despite the substantial weight loss achieved through bariatric surgery, patients face an increased risk of postoperative nutritional deficiencies over time, attributable to reduced food intake and malabsorption. According to the World Health Organization, one-third of the global population experiences some form of malnutrition, including micronutrient deficiencies, obesity, and diet-related non-communicable diseases. By 2025, half of the global population is projected to be malnourished []. Among individuals with obesity, both pre- and post-surgical nutritional deficiencies are prevalent, particularly in levels of vitamin D (VD), iron, transferrin (TRF) saturation, folic acid, hemoglobin (HGB), and parathyroid hormone. These deficiencies are influenced by factors such as the degree of obesity, ethnicity, geographic region, dietary culture, and sex []. Preoperatively, deficiencies in bariatric surgery candidates have been reported at rates ranging from 71%–100% for VD, 2.9% - 7.6% for zinc, 7% for ferritin (FER), 11.6% for TRF, 2.2% for HGB, and 1.1% - 13.4% for albumin (ALB) [-]. Postoperative deficiency rates vary significantly across studies of 24.3% - 100% for VD, 4.2% - 50% for ALB, 0% - 55% for FER, 4.7% - 8% for HGB, and 19% - 40% for zinc [,,]. Addressing nutritional deficiencies through preoperative assessment and correction is crucial, as such deficiencies can exacerbate postoperative nutrition-related complications.
Additionally, recent evidence indicates that obesity and its associated metabolic abnormalities significantly increase the risk for severe COVID-19 outcomes [,]. Bariatric surgery, by effectively reducing body weight and improving metabolic profiles, may indirectly enhance immune function and thus improve clinical outcomes in patients who contract SARS-CoV-2. Even COVID-19 associated treatment or vaccine have been invented, maintaining an adequate nutritional status is critical for optimal immune competence, whereas postoperative nutritional deficiencies could compromise host defenses against viral infections [,]. Therefore, the investigation of nutritional deficiencies and dietary pattern changes following bariatric surgery not only aids in optimizing postoperative management but also provides an indirect framework for understanding and potentially improving immune responses in high-risk obese populations during the COVID-19 pandemic.
Although several studies have examined macronutrient and micronutrient intake before and after bariatric surgery [-], the impact of dietary patterns on weight loss remains inadequately understood. Dietary patterns reflect individual eating habits and daily nutrient intake, and poor dietary habits are responsible for at least 8 million deaths annually []. Suboptimal dietary practices, including excessive sodium intake, insufficient fruit consumption, and high consumption of refined grains, have been associated with 1.51 million cardiometabolic deaths (51.0%) between 2010 and 2012 []. Therefore, evaluating dietary patterns is essential to understanding the etiology of obesity and its associated diseases [,].
113 Chinese adults (59.3% female, mean age 33.4 ± 9.79 years, mean BMI 37.04 ± 7.26 kg/m2) underwent laparoscopic bariatric surgery, of which 47.8% were sleeve gastrectomy with jejunal bypass (SGJB), 33.6% were SG and 18.6% were Roux-en-Y gastric bypass (RYGB). Patients completed baseline evaluation and follow-up in a tertiary hospital from 2018 to 2021. Bioelectrical impedance analysis (BIA) was used to assess the body composition information, including weight, BMI, waist-hip ratio, body fat ratio, skeletal muscle, and basal metabolic rate. Percent of total weight loss (% TWL) and % EWL were calculated three months after surgery. The biochemical data of each patient at baseline(M0) and three months after surgery(M3) were analyzed, including blood routine, liver function, renal function, 25-hydroxy vitamin D (25(OH)D), serum zinc, ALB, prealbumin (PA), retinol-binding protein (RBP), TRF, FER, and HGB. Other nutrients such as folic acid, vitamin B12 were not included in the analysis due to insufficient cases.
All patients completed Food Frequency Questionnaire (FFQ) and a 24-hour dietary record at M0 and M3. Nutritional assessment was conducted by a registered dietitian. The FFQ collected from Jinshazhou Hospital of Guangzhou University of Chinese Medicine was mainly composed of two parts. The first part includes information about appetite change, eating habits, gastrointestinal problems, etc. The second part includes 56 food items in 9 food groups: cereals, vegetables, fruit, meat, poultry, aquatic products, eggs, soybeans, milk and dairy products, and water. The questionnaire was designed with 6 response levels: never or less than 4 times a month, once a week, 2-4 times a week, 5-6 times a week, 1-2 times a day, more than 2 times a day. Validated photos, such as 60 g of an egg, and 200 g of an apple, were used to help quantify the intake of portion size. 110 valid questionnaires and 24-hour dietary records were collected. The weight in grams of each food was multiplied by its frequency of consumption. However, we did not calculate the intake of macronutrients, vitamins, and minerals.
After surgery, patients received oral nutritional supplements (ONS) to augment dietary protein intake and prevent malnutrition. In accordance with evidence-based guidelines, supplementation protocols were tailored by procedure type []. For example, patients undergoing SG and SGJB received ONS containing 231 kcal, 9.25 g protein, 28.2 g carbohydrates, and 9.1 g fat per serving, supplemented with chewable tablets containing vitamins and micronutrients (each tablet contains: vitamin A 375mcg, vitamin C 120 mg, VD 1000 IU, calcium carbonate and calcium citrate 600.84 mg, vitamin E 24.8 mg, vitamin B1 10 mg, vitamin B2 10 mg, vitamin B5 10 mg, vitamin B6 10 mg, vitamin B12 500 mg, folic acid 500 mg, niacin 50 mg, biotin 300 mcg, iron 18 mg,
magnesium 105 mg, iodine 150 mcg, copper 750 mcg, selenium 60 mcg, zinc 15 mg, manganese 2 mg, chromium
120 mcg, molybdenum 75 mcg, choline bitartrate 5 mg). Patients undergoing RYGB received similar supplementation adjusted for individual tolerance. Detailed protocols are provided in Supplementary Table 1.
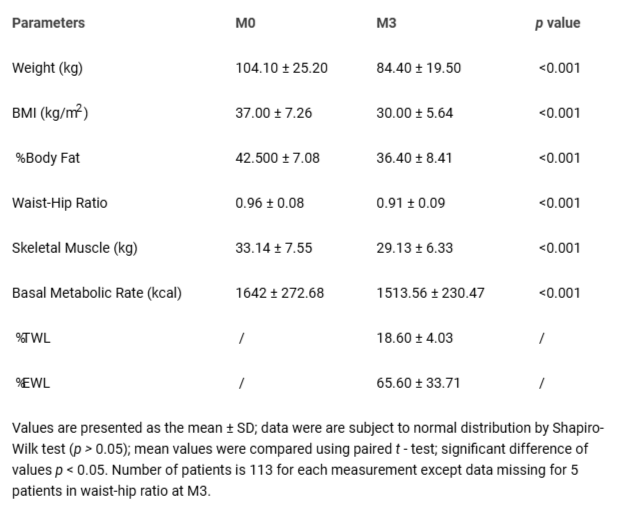 Table 1: Anthropometric characteristics at baseline (M0) and three months after bariatric surgery (M3).
Table 1: Anthropometric characteristics at baseline (M0) and three months after bariatric surgery (M3).Continuous variables are presented as mean with standard deviation (SD) and interquartile range (IQR) and frequencies as percentages. Paired t - test and chi-square test were used to analyze for continuous variables and categorical variables, respectively. Nonparametric tests (the Mann-Whitney U test and paired Wilcoxon rank-sum tests) were used to test the difference in various food intake frequencies before and after surgery; The Kruskal-Wallis test was used to test the difference in various food intake frequencies between three types of procedures. IBM SPSS Statistics 25.0 software was used and a p - value below 0.05 was considered to be significant.
Please See Supplementary Tables for additional data.
Bariatric surgeries are widely recognized for their long-term efficacy. Numerous studies have explored the physiological mechanisms underlying weight loss after bariatric surgery. Luo and Tavakkoli highlighted that weight loss involves a range of physiological mechanisms, including hormonal changes, improvements in immune function, alterations in bile acid signaling, enhanced hepatoportal glucose processing, and changes in the gut microbiome []. Baheeg, et al. reported a 90% satisfaction rate among patients who maintained an 18.88% total weight loss (TWL) five years post-surgery []. Maciejewski, et al. demonstrated that Roux-en-Y gastric bypass (RYGB) sustained long-term excess weight loss (%EWL) of 56.4%, with 71.8% of patients achieving >20% weight loss and 39.7% achieving >30% weight loss at 10 years postoperatively [].
As shown in Table 1, all three bariatric procedures—RYGB, sleeve gastrectomy (SG), and sleeve gastrectomy with jejunal bypass (SGJB)—significantly reduced patients’ weight (p < 0.05), accompanied by improvements in other key parameters, including BMI, % body fat, waist–hip ratio, skeletal muscle mass, and basal metabolic rate. Among the three procedures, a significant gender-based difference in BMI changes was observed only for SGJB (men: −8.822; women: −7.357; p < 0.05), as illustrated in Figure 1. Xu, et al. reported results consistent with our findings, noting a TWL of 18% and an EWL of 72% [].
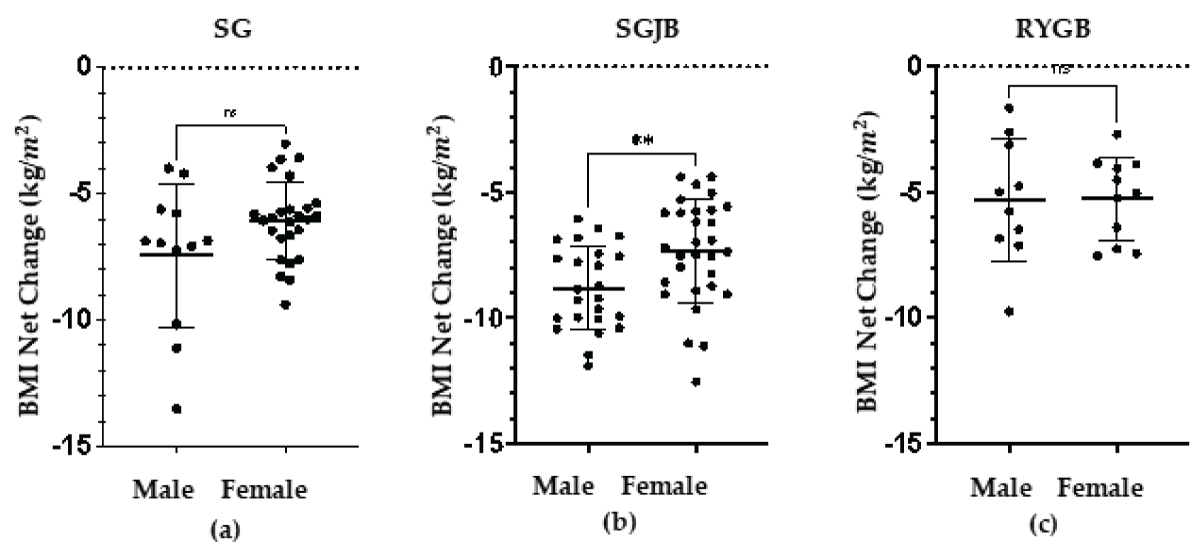 Figure 1: Net Change of BMI between men and women in three procedures. Among three procedure groups, significant difference in net change of BMI between men and women was only found in the SGJB group (p < 0.05).
Figure 1: Net Change of BMI between men and women in three procedures. Among three procedure groups, significant difference in net change of BMI between men and women was only found in the SGJB group (p < 0.05).While bariatric surgery provides substantial benefits in terms of weight loss, the risk of postoperative nutritional deficiencies increases over time due to inadequate dietary intake, indigestion, malabsorption, and drug–nutrient interactions. Serum proteins, including ALB, PA, RBP, and TRF, are crucial indicators for assessing nutritional status. As presented in Table 2 and Figure 2, the prevalence of PA and RBP deficiencies at M3 were significantly higher than at M0 (p < 0.001), whereas the incidence of ALB deficiency was lower at M3 than at M0 (p < 0.05). Celik, et al. linked low total protein and ALB levels to a heightened risk of malnutrition. However, ALB, as an acute negative reactant, can be influenced by confounding factors such as infection [].
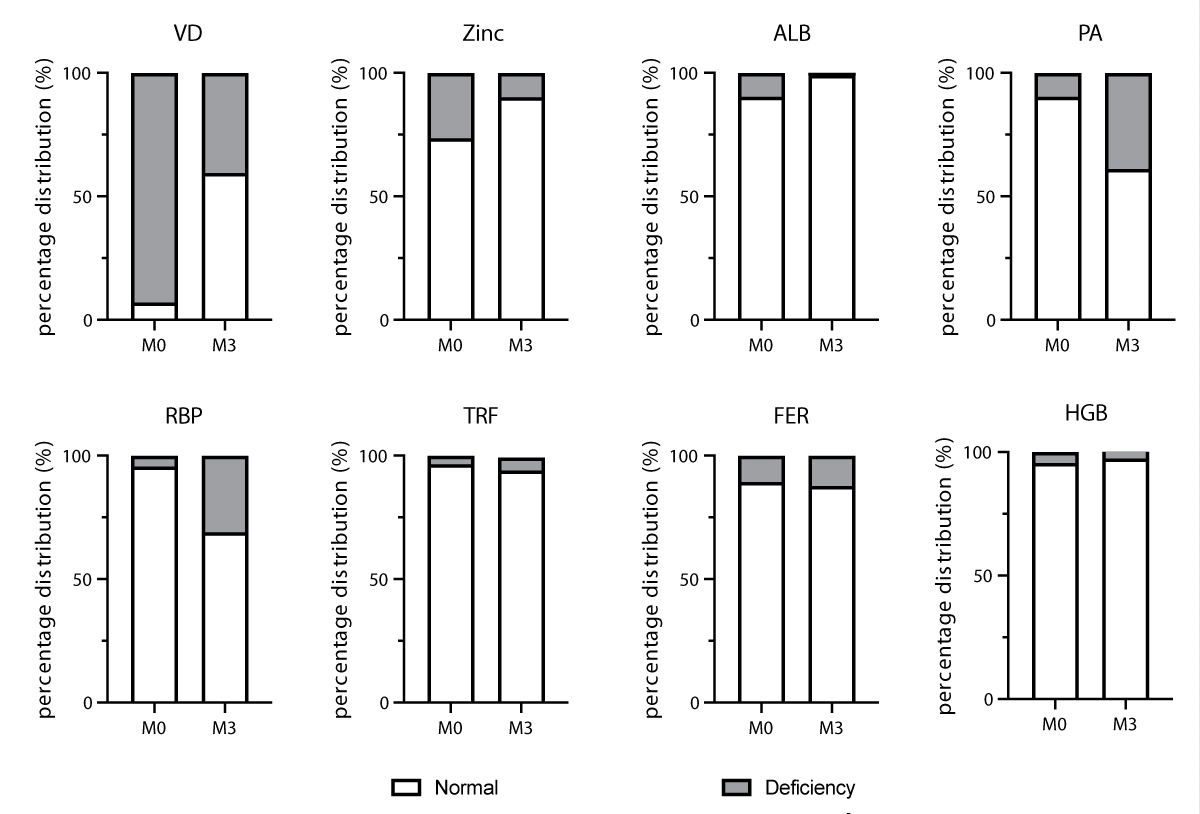 Figure 2: Patients’ percentage in nutritional deficiencies status (percentage distribution, %) of normal or deficiency before and 3 months after bariatric surgery (data from table 2). Dark gray: percentage of patients in normal nutritional status. Light gray: percentage of patients in Deficiency nutritional status.
Figure 2: Patients’ percentage in nutritional deficiencies status (percentage distribution, %) of normal or deficiency before and 3 months after bariatric surgery (data from table 2). Dark gray: percentage of patients in normal nutritional status. Light gray: percentage of patients in Deficiency nutritional status.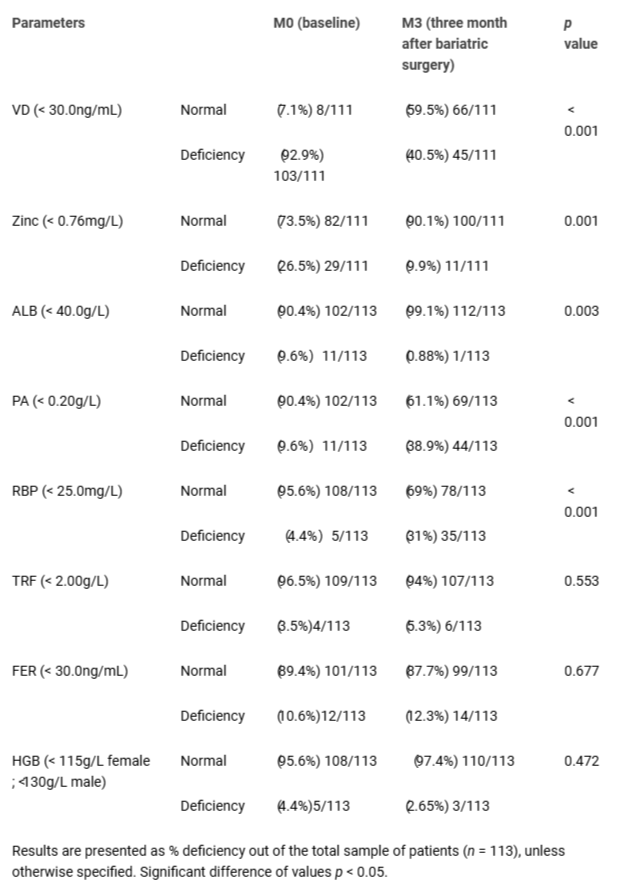 Table 2: Prevalence of nutritional deficiencies at baseline (M0) and three months after bariatric surgery (M3).
Table 2: Prevalence of nutritional deficiencies at baseline (M0) and three months after bariatric surgery (M3).RBP, with a half-life of 12 hours [], is the most responsive protein in the body, while PA, with a half-life of 2–3 days [] , is more sensitive in reflecting changes in nutritional status than TRF and ALB, which have half-lives of 8 and 20 days, respectively [,]. Protein deficiency, primarily caused by inadequate intake and malabsorption, manifests as muscle weakness, fragility, and edema [].
Vitamin D (VD) plays a pivotal role in bone health by maintaining calcium and phosphorus homeostasis, alongside its immunological and cardiovascular benefits []. Preoperative VD insufficiency and deficiency were prevalent in our study, consistent with prior research [,]. Parrott, et al. found postoperative VD deficiency in 100% of their patients. Key factors influencing VD levels include BMI, comorbidities, body fat percentage, sun exposure, postoperative physical activity, and lifestyle []. Chakhtoura, et al. recommended multivitamin supplementation with an additional 5000 IU of VD daily, combined with dietary interventions and sunlight exposure, as a single VD dose is insufficient for most patients to achieve normal 25(OH)D levels [,]. Our study revealed adherence rates to multivitamin supplementation of 62% (daily), 28.3% (sometimes), and 9.7% (never). High-dose VD3 supplementation (5000–6000 IU) significantly improved 25(OH)D levels at M3 (p < 0.001).
Iron is essential for immunometabolism and brain function [,]. Iron deficiency is common in individuals with obesity and chronic low-grade systemic inflammation, which impairs iron absorption and bioavailability []. Although bariatric surgery mitigates obesity-related complications and inflammation, malabsorption exacerbates iron deficiency. Gowanlock, et al [] observed a decline in ferritin (FER) levels from a peak at 3 months post-surgery. Factors contributing to iron deficiency and anemia include preoperative FER levels, malabsorptive procedures, and age.
According to the World Health Organization, useful biomarkers to assess iron status are serum FER and TRF saturation []. However, the level of FER can be elevated during malignancy and infection []. Benotti, et al. found that the rate of iron deficiency (approximately 60%) in metabolic surgery candidates may be underestimated when considering inflammation. The rate of iron deficiency may be two or three times higher than the prevalence of low FER []. Even though we instructed patients with FER concentrations of < 30 ng/L to take iron supplements (40–80 mg of Fe) and vitamin C, the prevalence of iron deficiency increased by 2.3% at M3 compared with the incidence at M0.
We found a significant difference in HGB levels at M3 (p < 0.05) compared with levels at M0 between the three bariatric procedures, as shown in Table 3. The RYGB group had a higher risk of anemia at M3 compared with the risk in the two other groups. Iron deficiency can be induced by the impaired absorption of iron owing to the reduction of gastric acid and the use of antacids [,]. Early diagnosis and intervention are strategies to prevent the development of iron deficiency and iron-deficiency anemia, which progress long-term after bariatric surgery []. Other nutrients related to anemia are vitamin B12 and folic acid, which are not routinely measured at M3 in our center. The prevalence of folic acid and vitamin B12 deficiencies is relatively low in the literature (at M0 and M3) [].
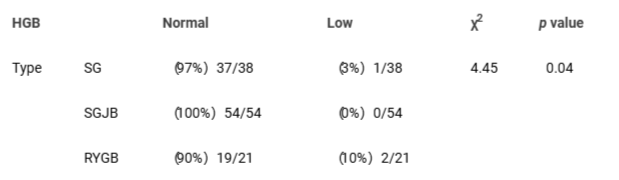 Table 3: Association between postoperative anemia and different types of surgery Between group differences for three procedures were analyzed by use of ANOVA and the χ² test.
Table 3: Association between postoperative anemia and different types of surgery Between group differences for three procedures were analyzed by use of ANOVA and the χ² test.Zinc is an important element of metalloenzymes and transcription factors in the body [,]. Zinc deficiency can lead to hair loss, diarrhea, anemia, and an altered sense of taste [,]. The preoperative prevalence of zinc deficiency in our study was higher than that in the literature [,]. The higher prevalence of zinc deficiency before surgery found in our study might be related to a relatively low intake of zinc-containing foods among patients living in inland cities of China. However, the prevalence of zinc deficiency at M3 was significantly lower (9.9%) than that at M0 (p < 0.05). Regarding supplementation, we advised patients to take zinc gluconate when serum zinc values were < 0.76 mg/L. Copper levels should be evaluated with long-term zinc supplementation because this can lead to copper deficiency [,].
A balanced diet not only meets a person’s energy and nutrient requirements but also helps maintain a healthy weight and prevent obesity and obesity-related comorbidities []. Dietary Guidelines for Chinese Residents (2022) and the CFP recommend ingesting at least 25 different foods each week, mainly plant-based foods, supplemented with animal-source foods []. Nevertheless, dietary imbalances were observed in China from 1961 to 2017: the consumption of whole grains and legumes in China declined annually over this period, accompanied by an increase in animal-source foods and processed foods [,]. The dietary patterns among the Chinese population are now similar to those in populations in Western countries []. Rising demand for sweetened beverages and convenience foods, as well as red meat and refined grains, is associated with stroke, coronary artery disease, and diabetes [,]. In contrast, the ingestion of fruit, vegetables, whole grains, skimmed dairy products, and fermented dairy products could prevent prediabetes [].
Even though a rich variety of foods is recommended after surgery, common complications, such as vomiting and abdominal bloating, can result in food restriction and further exacerbate existing nutritional deficiencies. A prospective observational study indicated that the food tolerance score and total energy intake decreased significantly 1 month after bariatric surgery but increased three months after surgery []. In addition, other studies found that in patients undergoing RYGB, energy intake decreased by 45% - 72%, and the intake of carbohydrate, protein, fat, and micronutrients also decreased (p < 0.001) [,].
In Chinese adults, 50%–60% of the total calorie intake comes from carbohydrates, mainly derived from refined grains [,]. Assessment of grain intake is particularly important to evaluate the dietary patterns among the Chinese population. The consumption of grain intake declined over the past 30 years; specifically, the intake of legumes was low []. The consumption of rice and wheat has different associations with metabolic syndrome between regions and genders [,]. At M3, the frequency of cereals, tubers, and legumes intake declined significantly after all three bariatric procedures (p < 0.001) as shown in Table 4. Most patients reported a sensation of “plugging” and an urge to vomit after eating rice and noodles during the first three months or even longer, postoperatively. Gastrointestinal complications might be a major cause of the reduction in carbohydrate intake. The intake of cereals, tubers, and legumes at M3 was substantially higher after RYGB than that after SG and SGJB (Table 5). Patients who underwent RYGB appeared to have a higher tolerance for cereals compared with the tolerance in patients who underwent SG or SGJB, even though some studies suggest that postoperative intake of monosaccharides leads to dumping syndrome and hypoglycemia []. The reduction of cereals, tubers, and legumes intake at M3 after bariatric surgery is a major factor in lowering the total energy intake and energy distribution ratio of carbohydrates []. Nevertheless, we did not find association between the number of cereals, tubers, and legumes consumption and weight loss. A study by Andromalos found no significant relationship between the energy distribution ratio of macronutrients and weight loss [].
The main dietary protein sources are meat, poultry, aquatic products, eggs, soybeans, and milk and dairy products, which provide complete protein, B vitamins, essential fatty acids, calcium, and other nutrients. The average intake of meat, poultry, and aquatic products at M0 was higher than the levels recommended by the CFP, whereas the intake of eggs, milk and dairy products, soybeans were comparatively low. The frequency of egg, milk and dairy products intake at M3 was significantly higher at M3 (p < 0.001) than that at M0. Despite the fact that plant-based proteins are recommended after bariatric surgery, the intake of soybean at M0 was comparable to that at M3. According to our dietary assessment, the reasons why patients consumed low amounts of high-quality protein were as follows: concerns regarding high cholesterol in eggs, milk-drinking habits, high purine in soybeans, insecure food sources, and time constraints and cost regarding cooking.
The intake of meat, poultry, and aquatic products decreased postoperatively. Tough and dry meat as an important source of protein was poorly tolerated early after bariatric surgery. Inadequate protein intake and malabsorption after bariatric surgery increase the risk of protein deficiency []. This deficiency leads to muscle loss, fatigue, hair loss [], and even edema, which exerts an influence on immune function and metabolism []. Medical nutrition therapy recommendations include a high protein intake of at least 60 g or 1.5 g/kg of ideal body weight after bariatric surgery []. In a study by Guillet, et al. [], spontaneous protein intake after surgery could not meet the protein requirements for most patients, even though the amount changed over time. During a 7-year follow-up study, postoperative protein intake was low, and in at least one-quarter of the subjects, the amount was below the recommended dietary limit []. Although postoperative protein powder supplementation helped increase the patients’ total protein intake, many patients experienced postoperative changes in their sense of taste, and gastrointestinal intolerance, which might have decreased their compliance with protein supplementation []. In our study, only 38.9% of the patients reported to take protein powder every day throughout three months as suggested, 36.3% of the patients reported sometimes, and 24.8% of the patients reported never.
As patients gradually adapt to the changes in dietary patterns and the limitations of obesity surgery, gastrointestinal symptoms are alleviated []. The frequency of intake of vegetables (p < 0.05) and fruit (p < 0.001) increased significantly at M3 compared with that at M0. Vegetables and fruit containing vitamins, minerals, dietary fiber, and phytochemicals are important parts of a healthy diet. Increasing the intake of fruit and vegetables can effectively reduce the risk of chronic diseases [,]. Continuous nutrition education, such as food choices, eating habits, and cooking tips, provided by a registered dietitian collaborating with a multidisciplinary team helps patients establish healthy dietary patterns.
Weight loss after bariatric surgery does not involve addressing energy intake and expenditure alone. Selecting specific dietary patterns like Jiangnan diet may have beneficial impacts on obesity management []. Future work is needed to investigate the relationships between eating patterns, eating behavior, and weight over time.
On the other hand, inner physiological system also plays a significant role as the microenvironment might be changed post-surgery. Biobaku, et al. (2020) claims that obesity and inflammation could be reversal with weight loss by surgery via cytokines regulation. Among those cytokines, CCL18 plays a role (downregulated) in all three types of surgeries (RYGB, SB, and AGB), which suggesting CCL18 might be critical in metabolism activities [-].
The strengths of this study are that we evaluated three different bariatric procedures; we reported the prevalence of nutritional deficiencies, nutritional supplementation dosage, and weight outcomes; and our findings were similar to those in previous studies. Although we did not calculate macronutrient and micronutrient intake, all patients in this study completed follow-up visits, and a 24-hour dietary record was used to validate dietary intake. However, a more comprehensive FFQ should be used to improve self-reported validity and reduce bias.
While our study demonstrates significant short-term improvements in anthropometric parameters and dietary modifications following bariatric surgery, the limited three-month follow-up period precludes an evaluation of the long-term sustainability of these changes. The limitation of this study was the small number of patients with certain nutritional deficiencies, such as vitamin B1, folic acid, vitamin B12, copper, and calcium due to extended intervals between follow-up visits. Additionally, we were unable to evaluate the patients’ compliance with nutritional supplementation and the durability of weight loss over a long period of time owing to a low rate of participation in follow-up visits. Future iterations of this work should consider extending the follow-up period to 12 months or beyond. Such extended monitoring would allow us to track whether the early improvements in nutritional markers and dietary habits are maintained over time or if deficiencies recur. Furthermore, our findings support the need for tailored, evidence-based supplementation protocols that differ according to the type of bariatric procedure.
In conclusion, bariatric surgery results in significant short-term weight loss and favorable changes in dietary patterns. However, the durability of these modifications remains uncertain due to the short follow-up period. Future studies should incorporate extended follow-up intervals to better understand long-term adherence to dietary modifications and the potential recurrence of nutritional deficiencies. Additionally, optimizing supplementation protocols based on procedure type may enhance clinical outcomes and patient adherence. These findings provide a foundation for future research aimed at improving postoperative nutritional management and long-term weight maintenance.
We are indebted to Prof. Liangping Wu and Xiaojiang Dai for their assistance. We also want to thank Ruiqi Wang for illustrating the graphical abstract.
XW and CP were major contributors in writing the manuscript. YT analyzed and interpreted the patient data regarding the anthropometric parameters, biochemical data and eating patterns. NH organized and reviewed manuscript. All authors read and approved the final manuscript.
The data that support the findings of this study are available from Jinshazhou Hospital of Guangzhou University of Chinese Medicine but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of Jinshazhou Hospital of Guangzhou University of Chinese Medicine. Please contact the corresponding author (Yuebin TAN), if individuals want to request the data from this study.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the ethic committee of Jinshazhou Hospital of Guangzhou University of Chinese Medicine [JSZ-IEC-SL-KT-20220418(1)] and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
World Health Organization. "WHO Accelerates Work on Nutrition Targets with New commitments 2021[Available from: https://www.who.int/news/item/07-12-2021-who-accelerates-work-on-nutrition-targets-with-new-commitments.
Pan XF, Wang L, Pan A. Epidemiology and determinants of obesity in China. Lancet Diabetes Endocrinol. 2021 Jun;9(6):373-392. doi: 10.1016/S2213-8587(21)00045-0. Erratum in: Lancet Diabetes Endocrinol. 2021 Jul;9(7):e2. doi: 10.1016/S2213-8587(21)00149-2. PMID: 34022156.
GBD 2015 Obesity Collaborators; Afshin A, Forouzanfar MH, Reitsma MB, Sur P, Estep K, Lee A, et al. Health Effects of Overweight and Obesity in 195 Countries over 25 Years. N Engl J Med. 2017 Jul 6;377(1):13-27. doi: 10.1056/NEJMoa1614362. Epub 2017 Jun 12. PMID: 28604169; PMCID: PMC5477817.
Albaugh VL, Kindel TL, Nissen SE, Aminian A. Cardiovascular Risk Reduction Following Metabolic and Bariatric Surgery. Surg Clin North Am. 2021 Apr;101(2):269-294. doi: 10.1016/j.suc.2020.12.012. PMID: 33743969.
Fischer H, Weiss RE, Friedman AN, Imam TH, Coleman KJ. The relationship between kidney function and body mass index before and after bariatric surgery in patients with chronic kidney disease. Surg Obes Relat Dis. 2021 Mar;17(3):508-515. doi: 10.1016/j.soard.2020.11.010. Epub 2020 Nov 19. PMID: 33358080; PMCID: PMC7904605.
Wei Y, Wu T, Tong DKH, Law BTT, Leung DKW, Lam CLK, Wong CKH. Improvement in patient-reported outcomes in Chinese adults after bariatric surgery: 1-year follow-up of a prospective cohort. Surg Obes Relat Dis. 2020 Oct;16(10):1563-1572. doi: 10.1016/j.soard.2020.04.050. Epub 2020 May 15. PMID: 32675022.
The American Society for Metabolic & Bariatric Surgery. 2021 20 April 2022]; Available from: https://asmbs.org/resources/metabolic-and-bariatric-surgery.
Yue TP, Mohd Yusof BN, Nor Hanipah ZB, Gee T. Food tolerance, nutritional status and health-related quality of life of patients with morbid obesity after bariatric surgery. Clin Nutr ESPEN. 2022 Apr;48:321-328. doi: 10.1016/j.clnesp.2022.01.026. Epub 2022 Jan 31. PMID: 35331508.
Mohapatra S, Gangadharan K, Pitchumoni CS. Malnutrition in obesity before and after bariatric surgery. Dis Mon. 2020 Feb;66(2):100866. doi: 10.1016/j.disamonth.2019.06.008. Epub 2019 Jul 10. PMID: 31301800.
Emile, S.H., Elfeki,H, Nutritional Deficiency After Sleeve Gastrectomy: A Comprehensive Literature Review. EMJ Gastroenterol, 2017. 6(1): p. 99-105.
Guan B, Yang J, Chen Y, Yang W, Wang C. Nutritional Deficiencies in Chinese Patients Undergoing Gastric Bypass and Sleeve Gastrectomy: Prevalence and Predictors. Obes Surg. 2018 Sep;28(9):2727-2736. doi: 10.1007/s11695-018-3225-9. PMID: 29754386.
Collazo-Clavell ML, Shah M. Common and Rare Complications of Bariatric Surgery. Endocrinol Metab Clin North Am. 2020 Jun;49(2):329-346. doi: 10.1016/j.ecl.2020.02.003. Epub 2020 Apr 16. PMID: 32418594.
Tan BC, Park YS, Won Y, Lee S, Kang SH, Ahn SH, Park DJ, Kim HH. Preoperative Nutritional Deficiencies in Bariatric Surgery Candidates in Korea. Obes Surg. 2021 Jun;31(6):2660-2668. doi: 10.1007/s11695-021-05318-9. Epub 2021 Mar 8. PMID: 33686579.
Mechanick JI, Apovian C, Brethauer S, Garvey WT, Joffe AM, Kim J, et al. Clinical Practice Guidelines For The Perioperative Nutrition, Metabolic, And Nonsurgical Support Of Patients Undergoing Bariatric Procedures - 2019 Update: Cosponsored By American Association Of Clinical Endocrinologists/American College Of Endocrinology, The Obesity Society, American Society For Metabolic & Bariatric Surgery, Obesity Medicine Association, And American Society Of Anesthesiologists - Executive Summary. Endocr Pract. 2019 Dec;25(12):1346-1359. doi: 10.4158/GL-2019-0406. Epub 2019 Nov 4. PMID: 31682518.
Popkin BM, Du S, Green WD, Beck MA, Algaith T, Herbst CH, Alsukait RF, Alluhidan M, Alazemi N, Shekar M. Individuals with obesity and COVID-19: A global perspective on the epidemiology and biological relationships. Obes Rev. 2020 Nov;21(11):e13128. doi: 10.1111/obr.13128. Epub 2020 Aug 26. Erratum in: Obes Rev. 2021 Oct;22(10):e13305. doi: 10.1111/obr.13305. PMID: 32845580; PMCID: PMC7461480.
Simonnet A, Chetboun M, Poissy J, Raverdy V, Noulette J, Duhamel A, Labreuche J, Mathieu D, Pattou F, Jourdain M; LICORN and the Lille COVID-19 and Obesity study group. High Prevalence of Obesity in Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2) Requiring Invasive Mechanical Ventilation. Obesity (Silver Spring). 2020 Jul;28(7):1195-1199. doi: 10.1002/oby.22831. Epub 2020 Jun 10. Erratum in: Obesity (Silver Spring). 2020 Oct;28(10):1994. doi: 10.1002/oby.23006. PMID: 32271993; PMCID: PMC7262326.
Calder PC. Nutrition, immunity and COVID-19. BMJ Nutr Prev Health. 2020 May 20;3(1):74-92. doi: 10.1136/bmjnph-2020-000085. PMID: 33230497; PMCID: PMC7295866.
Lai NZ, Tan Y, Wang Y. Compositions and methods for treating COVID-19. United States; 2023.
Aron-Wisnewsky J, Verger EO, Bounaix C, Dao MC, Oppert JM, Bouillot JL, Chevallier JM, Clément K. Nutritional and Protein Deficiencies in the Short Term following Both Gastric Bypass and Gastric Banding. PLoS One. 2016 Feb 18;11(2):e0149588. doi: 10.1371/journal.pone.0149588. PMID: 26891123; PMCID: PMC4758752.
Raatz SK, Johnson LK, Caliquary A, King WC, Kalarchian MA, Devlin MJ, Marcus MD, Mitchell JE. Reported nutrient intake over 7 years after Roux-en-Y gastric bypass in the Longitudinal Assessment of Bariatric Surgery-3 (LABS-3) psychosocial study. Surg Obes Relat Dis. 2020 Aug;16(8):1022-1029. doi: 10.1016/j.soard.2020.04.007. Epub 2020 Apr 22. PMID: 32418771; PMCID: PMC7423730.
Calleja-Fernández A, Pintor-de-la-Maza B, Diez-Rodríguez R, Vidal-Casariego A, Urioste-Fondo A, Cano-Rodríguez I, Ballesteros-Pomar MD. Relationship Between Diet and Body Composition After Biliopancreatic Diversion. Obes Surg. 2015 Nov;25(11):2093-9. doi: 10.1007/s11695-015-1658-y. PMID: 26055550.
He Y, Li Y, Yang X, Hemler EC, Fang Y, Zhao L, Zhang J, Yang Z, Wang Z, He L, Sun J, Wang DD, Wang J, Piao J, Liang X, Ding G, Hu FB. The dietary transition and its association with cardiometabolic mortality among Chinese adults, 1982-2012: a cross-sectional population-based study. Lancet Diabetes Endocrinol. 2019 Jul;7(7):540-548. doi: 10.1016/S2213-8587(19)30152-4. Epub 2019 May 10. PMID: 31085143; PMCID: PMC7269053.
Rasaei N, Kashavarz SA, Yekaninejad MS, Mirzaei K. The association between sarcopenic obesity (SO) and major dietary patterns in overweight and obese adult women. Diabetes Metab Syndr. 2019 Jul-Aug;13(4):2519-2524. doi: 10.1016/j.dsx.2019.06.023. Epub 2019 Jul 9. PMID: 31405671.
Roman G, Rusu A, Graur M, Creteanu G, Morosanu M, Radulian G, Amorin P, Timar R, Pircalaboiu L, Bala C. DIETARY PATTERNS AND THEIR ASSOCIATION WITH OBESITY: A CROSS-SECTIONAL STUDY. Acta Endocrinol (Buchar). 2019 Jan-Mar;-5(1):86-95. doi: 10.4183/aeb.2019.86. PMID: 31149065; PMCID: PMC6535323.
Luo JN, Tavakkoli A. Physiologic Mechanisms of Weight Loss Following Metabolic/Bariatric Surgery. Surg Clin North Am. 2021 Apr;101(2):223-237. doi: 10.1016/j.suc.2020.12.006. PMID: 33743966.
Baheeg M, El-Din MT, Labib MF, Elgohary SA, Hasan A. Long-term durability of weight loss after bariatric surgery: a retrospective study. Int J Surg Open. 2021;28:37-40.
Maciejewski ML, Arterburn DE, Van Scoyoc L, Smith VA, Yancy WS Jr, Weidenbacher HJ, Livingston EH, Olsen MK. Bariatric Surgery and Long-term Durability of Weight Loss. JAMA Surg. 2016 Nov 1;151(11):1046-1055. doi: 10.1001/jamasurg.2016.2317. PMID: 27579793; PMCID: PMC5112115.
Xu T, Wang C, Zhang H, Han X, Liu W, Han J, Yu H, Chen J, Zhang P, Di J. Timing of Maximal Weight Reduction Following Bariatric Surgery: A Study in Chinese Patients. Front Endocrinol (Lausanne). 2020 Sep 15;11:615. doi: 10.3389/fendo.2020.00615. PMID: 33042006; PMCID: PMC7522214.
Celik ZM, Islamoglu AH, Sabuncular G, Toprak HS, Gunes FE. Evaluation of malnutrition risk of inpatients in a research and training hospital: A cross-sectional study. Clin Nutr ESPEN. 2021 Feb;41:261-267. doi: 10.1016/j.clnesp.2020.12.002. Epub 2020 Dec 23. PMID: 33487274.
Sensi M, Bruno MR, Valente L, Cioccia GP, Chianelli M, Pozzilli P. Retinol binding protein: a short half life determinant of protein non enzymatic glycation in diabetes. Diabetes Res. 1990 Apr;13(4):195-8. PMID: 2134212.
Li JD, Diao YK, Li J, Wu H, Sun LY, Gu WM, Wang H, Chen TH, Zeng YY, Zhou YH, Wang Y, Zhang YM, Liang YJ, Lau WY, Li C, Liang L, Wang MD, Zhang CW, Shen F, Shao CH, Yang T. Association between preoperative prealbumin level and postoperative mortality and morbidity after hepatic resection for hepatocellular carcinoma: A multicenter study from a HBV-endemic area. Am J Surg. 2021 May;221(5):1024-1032. doi: 10.1016/j.amjsurg.2020.08.036. Epub 2020 Sep 2. PMID: 32951853.
Neyra NR, Hakim RM, Shyr Y, Ikizler TA. Serum transferrin and serum prealbumin are early predictors of serum albumin in chronic hemodialysis patients. J Ren Nutr. 2000 Oct;10(4):184-90. doi: 10.1053/jren.2000.16325. PMID: 11070145.
Gomme PT, McCann KB, Bertolini J. Transferrin: structure, function and potential therapeutic actions. Drug Discov Today. 2005 Feb 15;10(4):267-73. doi: 10.1016/S1359-6446(04)03333-1. PMID: 15708745.
Faria SL, Faria OP, Buffington C, de Almeida Cardeal M, Ito MK. Dietary protein intake and bariatric surgery patients: a review. Obes Surg. 2011 Nov;21(11):1798-805. doi: 10.1007/s11695-011-0441-y. PMID: 21590346.
de la Guía-Galipienso F, Martínez-Ferran M, Vallecillo N, Lavie CJ, Sanchis-Gomar F, Pareja-Galeano H. Vitamin D and cardiovascular health. Clin Nutr. 2021 May;40(5):2946-2957. doi: 10.1016/j.clnu.2020.12.025. Epub 2020 Dec 29. PMID: 33397599; PMCID: PMC7770490.
Krzizek EC, Brix JM, Herz CT, Kopp HP, Schernthaner GH, Schernthaner G, Ludvik B. Prevalence of Micronutrient Deficiency in Patients with Morbid Obesity Before Bariatric Surgery. Obes Surg. 2018 Mar;28(3):643-648. doi: 10.1007/s11695-017-2902-4. PMID: 28849358.
Parrott J, Frank L, Rabena R, Craggs-Dino L, Isom KA, Greiman L. American Society for Metabolic and Bariatric Surgery Integrated Health Nutritional Guidelines for the Surgical Weight Loss Patient 2016 Update: Micronutrients. Surg Obes Relat Dis. 2017 May;13(5):727-741. doi: 10.1016/j.soard.2016.12.018. Epub 2017 Jan 19. PMID: 28392254.
Chakhtoura MT, Nakhoul N, Akl EA, Mantzoros CS, El Hajj Fuleihan GA. Guidelines on vitamin D replacement in bariatric surgery: Identification and systematic appraisal. Metabolism. 2016 Apr;65(4):586-97. doi: 10.1016/j.metabol.2015.12.013. Epub 2016 Jan 4. PMID: 26833101; PMCID: PMC4792722.
Chakhtoura MT, Nakhoul NN, Shawwa K, Mantzoros C, El Hajj Fuleihan GA. Hypovitaminosis D in bariatric surgery: A systematic review of observational studies. Metabolism. 2016 Apr;65(4):574-85. doi: 10.1016/j.metabol.2015.12.004. Epub 2015 Dec 19. PMID: 26805016; PMCID: PMC4792683.
Cronin SJF, Woolf CJ, Weiss G, Penninger JM. The Role of Iron Regulation in Immunometabolism and Immune-Related Disease. Front Mol Biosci. 2019 Nov 22;6:116. doi: 10.3389/fmolb.2019.00116. PMID: 31824960; PMCID: PMC6883604.
Wenger MJ, Rhoten SE, Murray-Kolb LE, Scott SP, Boy E, Gahutu JB, Haas JD. Changes in Iron Status Are Related to Changes in Brain Activity and Behavior in Rwandan Female University Students: Results from a Randomized Controlled Efficacy Trial Involving Iron-Biofortified Beans. J Nutr. 2019 Apr 1;149(4):687-697. doi: 10.1093/jn/nxy265. PMID: 30926992; PMCID: PMC6461719.
Bjørklund G, Peana M, Pivina L, Dosa A, Aaseth J, Semenova Y, Chirumbolo S, Medici S, Dadar M, Costea DO. Iron Deficiency in Obesity and after Bariatric Surgery. Biomolecules. 2021 Apr 21;11(5):613. doi: 10.3390/biom11050613. PMID: 33918997; PMCID: PMC8142987.
Gowanlock Z, Lezhanska A, Conroy M, Crowther M, Tiboni M, Mbuagbaw L, Siegal DM. Iron deficiency following bariatric surgery: a retrospective cohort study. Blood Adv. 2020 Aug 11;4(15):3639-3647. doi: 10.1182/bloodadvances.2020001880. PMID: 32766854; PMCID: PMC7422111.
WHO guideline on use of ferritin concentrations to assess iron status in individuals and populations. 2020; Available from: https://www.who.int/publications/i/item/9789240000124.
C-reactive protein concentrations as a marker of inflammation or infection for interpreting biomarkers of micronutrient status. 2014 20 April 2022]; Available from: https://www.who.int/publications/i/item/WHO-NMH-NHD-EPG-14.7.
Benotti PN, Wood GC, Kaberi-Otarod J, Still CD, Gerhard GS, Bistrian BR. New concepts in the diagnosis and management approach to iron deficiency in candidates for metabolic surgery: should we change our practice? Surg Obes Relat Dis. 2020 Dec;16(12):2074-2081. doi: 10.1016/j.soard.2020.08.018. Epub 2020 Aug 27. PMID: 33011074; PMCID: PMC7704546.
Zhang C, Chen X, Li J, Liu Z, Liu W, Zhang J, Zhou Z. Anaemia and Related Nutritional Deficiencies in Chinese Patients with Obesity, 12 Months Following Laparoscopic Sleeve Gastrectomy. Diabetes Metab Syndr Obes. 2021 Apr 12;14:1575-1587. doi: 10.2147/DMSO.S303320. PMID: 33880047; PMCID: PMC8051959.
Kambe T. Metalation and Maturation of Zinc Ectoenzymes: A Perspective. Biochemistry. 2020 Jan 14;59(1):74-79. doi: 10.1021/acs.biochem.9b00924. Epub 2019 Nov 26. PMID: 31718170.
Gilbert R, Peto T, Lengyel I, Emri E. Zinc Nutrition and Inflammation in the Aging Retina. Mol Nutr Food Res. 2019 Aug;63(15):e1801049. doi: 10.1002/mnfr.201801049. Epub 2019 Jun 27. PMID: 31148351.
Mahawar KK, Bhasker AG, Bindal V, Graham Y, Dudeja U, Lakdawala M, Small PK. Zinc Deficiency after Gastric Bypass for Morbid Obesity: a Systematic Review. Obes Surg. 2017 Feb;27(2):522-529. doi: 10.1007/s11695-016-2474-8. PMID: 27885534.
Osadchuk LV, Danilenko AD, Osadchuk AV. [An influence of zinc on male infertility]. Urologiia. 2021 Nov;(5):84-93. Russian. PMID: 34743439.
Soheilipour F, Ebrahimian M, Pishgahroudsari M, Hajian M, Amirkashani D, Ordooei M, Radgoodarzi M, Eskandari D. The prevalence of zinc deficiency in morbidly obese patients before and after different types of bariatric surgery. BMC Endocr Disord. 2021 May 25;21(1):107. doi: 10.1186/s12902-021-00763-0. PMID: 34030687; PMCID: PMC8147400.
Duncan A, Talwar D, Morrison I. The predictive value of low plasma copper and high plasma zinc in detecting zinc-induced copper deficiency. Ann Clin Biochem. 2016 Sep;53(Pt 5):575-9. doi: 10.1177/0004563215620821. Epub 2015 Nov 19. PMID: 26586851.
Kang S, Seo H, Moon HS, Kwon JH, Park YS, Yun CW. The Role of Zinc in Copper Homeostasis of Aspergillus fumigatus. Int J Mol Sci. 2020 Oct 16;21(20):7665. doi: 10.3390/ijms21207665. PMID: 33081273; PMCID: PMC7593903.
Chinese Nutrition Society, Dietary Guidelines for Chinese Residents(2022). 1st ed. 2022, Beijing, China: People's Medical Publishing House. 303-311.
Han A, Sun T, Ming J, Chai L, Liao X. Are the Chinese Moving toward a Healthy Diet? Evidence from Macro Data from 1961 to 2017. Int J Environ Res Public Health. 2020 Jul 23;17(15):5294. doi: 10.3390/ijerph17155294. PMID: 32717812; PMCID: PMC7432933.
Popkin BM. Synthesis and implications: China's nutrition transition in the context of changes across other low- and middle-income countries. Obes Rev. 2014 Jan;15 Suppl 1(0 1):60-7. doi: 10.1111/obr.12120. PMID: 24341759; PMCID: PMC3869101.
Siddiqui S, Zainal H, Harun SN, Sheikh Ghadzi SM. Dietary assessment of pre-diabetic patients by using food frequency questionnaire. A systematic review of study quality, study outcome, study questionnaire and their relative validity and reliability. Clin Nutr ESPEN. 2019 Feb;29:213-223. doi: 10.1016/j.clnesp.2018.10.002. Epub 2018 Nov 8. PMID: 30661689.
Schafer AL, Weaver CM, Black DM, Wheeler AL, Chang H, Szefc GV, Stewart L, Rogers SJ, Carter JT, Posselt AM, Shoback DM, Sellmeyer DE. Intestinal Calcium Absorption Decreases Dramatically After Gastric Bypass Surgery Despite Optimization of Vitamin D Status. J Bone Miner Res. 2015 Aug;30(8):1377-85. doi: 10.1002/jbmr.2467. Epub 2015 May 21. PMID: 25640580; PMCID: PMC4593653.
Ju L, Yu D, Fang H, Guo Q, Xu X, Li S, Zhao L. [Trends and food sources composition of energy, protein and fat in Chinese residents, 1992-2012]. Wei Sheng Yan Jiu. 2018 Sep;47(5):689-704. Chinese. PMID: 30593290.
Huang L, Wang H, Wang Z, Zhang J, Zhang B, Ding G. Regional Disparities in the Association between Cereal Consumption and Metabolic Syndrome: Results from the China Health and Nutrition Survey. Nutrients. 2019 Apr 1;11(4):764. doi: 10.3390/nu11040764. PMID: 30939825; PMCID: PMC6521195.
Cheng M, Wang H, Wang Z, Du W, Ouyang Y, Zhang B. Relationship between dietary factors and the number of altered metabolic syndrome components in Chinese adults: a cross-sectional study using data from the China Health and Nutrition Survey. BMJ Open. 2017 May 29;7(5):e014911. doi: 10.1136/bmjopen-2016-014911. PMID: 28554922; PMCID: PMC5729973.
Kushner RF, Cummings S, Herron DM. Bariatric surgery: postoperative nutritional management. 2020.
Andromalos L, Crowley N, Brown J, Craggs-Dino L, Handu D, Isom K, Lynch A, DellaValle D. Nutrition Care in Bariatric Surgery: An Academy Evidence Analysis Center Systematic Review. J Acad Nutr Diet. 2019 Apr;119(4):678-686. doi: 10.1016/j.jand.2018.08.002. Epub 2018 Nov 1. PMID: 30391396.
Ledoux S, Flamant M, Calabrese D, Bogard C, Sami O, Coupaye M. What Are the Micronutrient Deficiencies Responsible for the Most Common Nutritional Symptoms After Bariatric Surgery? Obes Surg. 2020 May;30(5):1891-1897. doi: 10.1007/s11695-020-04412-8. PMID: 31960214.
Stocker R, Ceyhan M, Schönenberger KA, Stanga Z, Reber E. Nutrient and fluid requirements in post-bariatric patients performing physical activity: A systematic review. Nutrition. 2022 May;97:111577. doi: 10.1016/j.nut.2021.111577. Epub 2021 Dec 24. PMID: 35248847.
Guillet C, Masgrau A, Mishellany-Dutour A, Blot A, Caille A, Lyon N, Pereira B, Slim K, Robert M, Disse E, Feugier N, Le Ruyet P, Louvet C, Miolanne M, Farigon N, Laville M, Boirie Y. Bariatric surgery affects obesity-related protein requirements. Clin Nutr ESPEN. 2020 Dec;40:392-400. doi: 10.1016/j.clnesp.2020.06.007. Epub 2020 Oct 1. PMID: 33183568.
Hirsch KR, Blue MNM, Trexler ET, Ahuja S, Smith-Ryan AE. Provision of ready-to-drink protein following bariatric surgery: An evaluation of tolerability, body composition, and metabolic rate. Clin Nutr. 2021 Apr;40(4):2319-2327. doi: 10.1016/j.clnu.2020.10.022. Epub 2020 Oct 23. PMID: 33158590.
Barnard J, Snowdon D, Hewitson L. Dietary interventions for weight loss and essential aspects of nutrition post–bariatric surgery. In: Practical Guide to Obesity Medicine. 2018;315-327.
Zurbau A, Au-Yeung F, Blanco Mejia S, Khan TA, Vuksan V, Jovanovski E, Leiter LA, Kendall CWC, Jenkins DJA, Sievenpiper JL. Relation of Different Fruit and Vegetable Sources With Incident Cardiovascular Outcomes: A Systematic Review and Meta-Analysis of Prospective Cohort Studies. J Am Heart Assoc. 2020 Oct 20;9(19):e017728. doi: 10.1161/JAHA.120.017728. Epub 2020 Oct 1. PMID: 33000670; PMCID: PMC7792377.
Wang J, Lin X, Bloomgarden ZT, Ning G. The Jiangnan diet, a healthy diet pattern for Chinese. J Diabetes. 2020 May;12(5):365-371. doi: 10.1111/1753-0407.13015. Epub 2020 Jan 26. PMID: 31846221; PMCID: PMC7216939.
Biobaku F, Ghanim H, Monte SV, Caruana JA, Dandona P. Bariatric Surgery: Remission of Inflammation, Cardiometabolic Benefits, and Common Adverse Effects. J Endocr Soc. 2020 Aug 4;4(9):bvaa049. doi: 10.1210/jendso/bvaa049. PMID: 32775937; PMCID: PMC7402590.
Tan Y, Mo Y, Lai NZ. CCL18 induces healthy fibroblast-like synoviocytes to develop gene expression profiling similar to fibroblast-like synoviocytes of rheumatoid arthritis. Cytokines 2020 Virtual Meeting – Abstract Book. 2020:60-61.
Tan Y, Mo Y, Lai NZ. PITPMN3 is a potential gene therapy target to treat rheumatoid arthritis in fibroblast-like synoviocytes by inhibiting CCL18 associated effect, which might activate Toll-like receptor pathway. Mol Ther. 2021;29(4):368.
Tan Y, Hu N, Wu X. The role of CCL18 in rheumatoid arthritis diseases. IgMin Res. 2025;3(1):021-026.
Wu X, Pan C, Han N, Tan Y. Risk of Nutritional Deficiencies and Changes in Dietary Patterns after Bariatric Surgery. IgMin Res. April 01, 2025; 3(4): 133-141. IgMin ID: igmin293; DOI:10.61927/igmin293; Available at: igmin.link/p293
Anyone you share the following link with will be able to read this content:
1Surgical Center for Obesity and Diabetes, Jinshazhou Hospital of Guangzhou University of Chinese Medicine, Guangdong 510168, China
2Faculty of Education, The University of Hong Kong, HKSAR, China
3Department of Biochemistry and Molecular and Cellular Biology, Georgetown University, Washington, DC 20007, United States
Address Correspondence:
Yuebin Tan, Department of Biochemistry and Molecular and Cellular Biology, Georgetown University, Washington, DC 20007, United States, Email: ty157@georgetown.edu
How to cite this article:
Wu X, Pan C, Han N, Tan Y. Risk of Nutritional Deficiencies and Changes in Dietary Patterns after Bariatric Surgery. IgMin Res. April 01, 2025; 3(4): 133-141. IgMin ID: igmin293; DOI:10.61927/igmin293; Available at: igmin.link/p293
Copyright: © 2025 Wu X, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
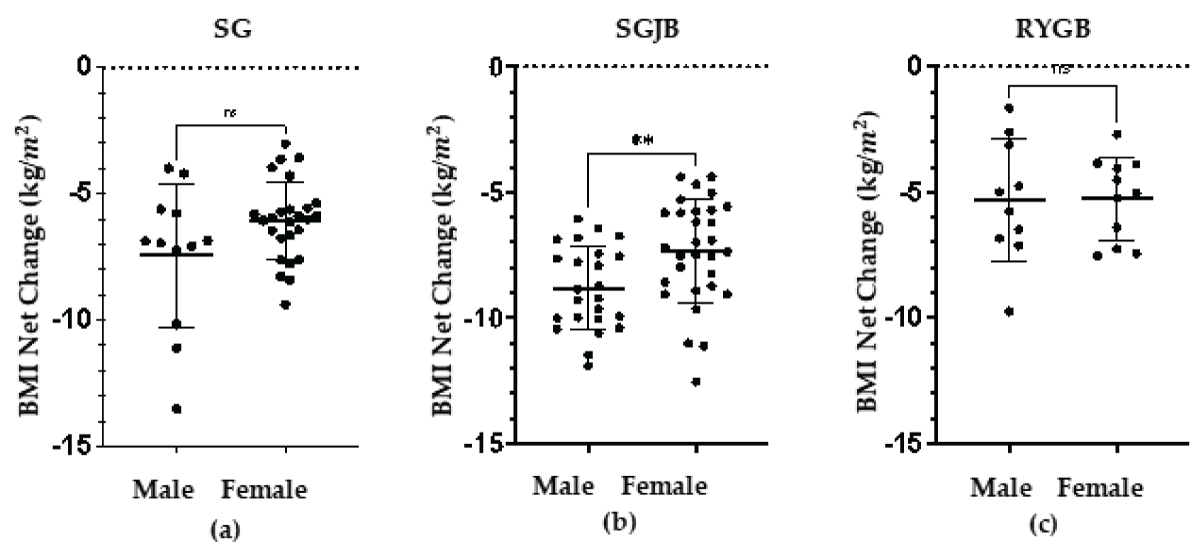 Figure 1: Net Change of BMI between men and women in three p...
Figure 1: Net Change of BMI between men and women in three p...
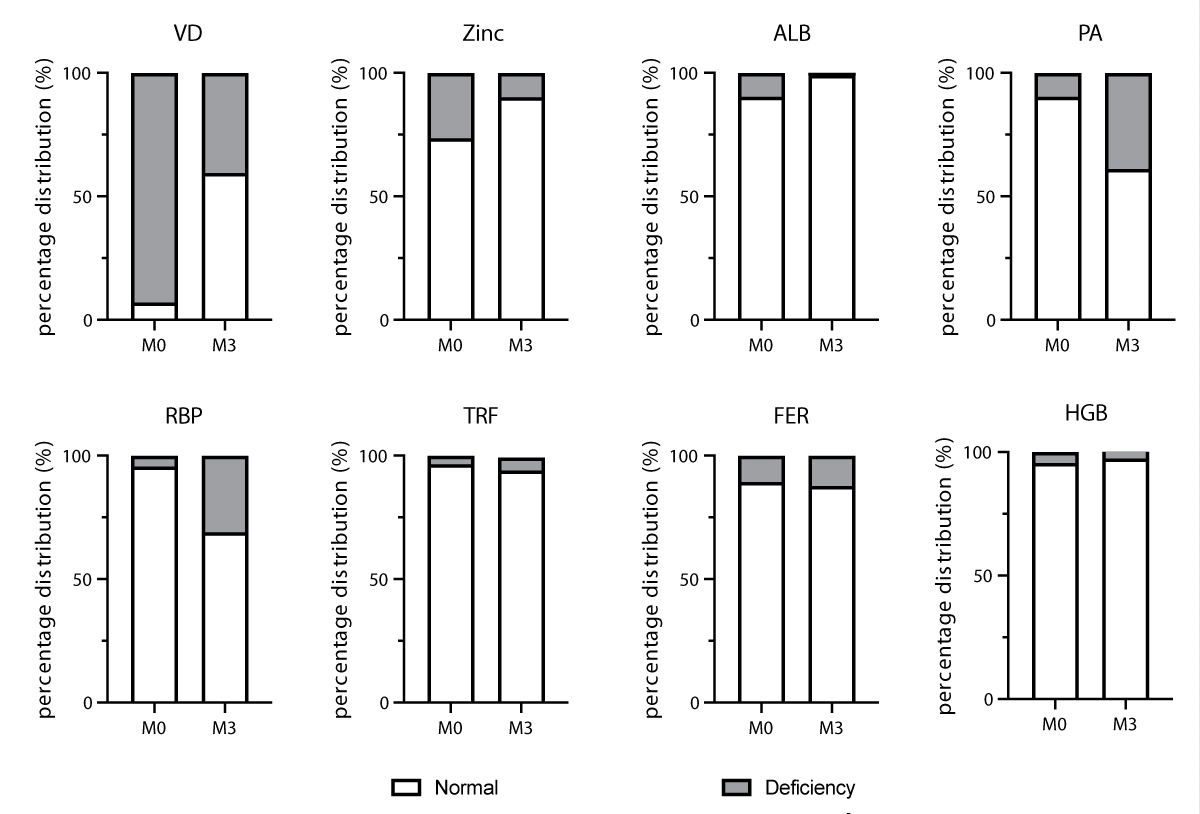 Figure 2: Patients’ percentage in nutritional deficiencies...
Figure 2: Patients’ percentage in nutritional deficiencies...
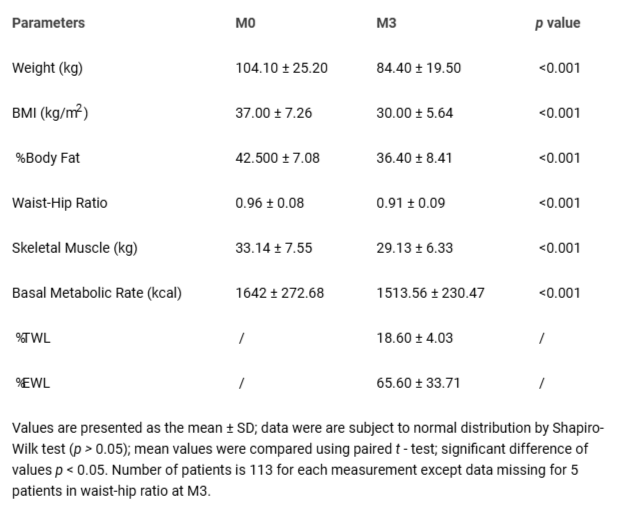 Table 1: Anthropometric characteristics at baseline (M0) an...
Table 1: Anthropometric characteristics at baseline (M0) an...
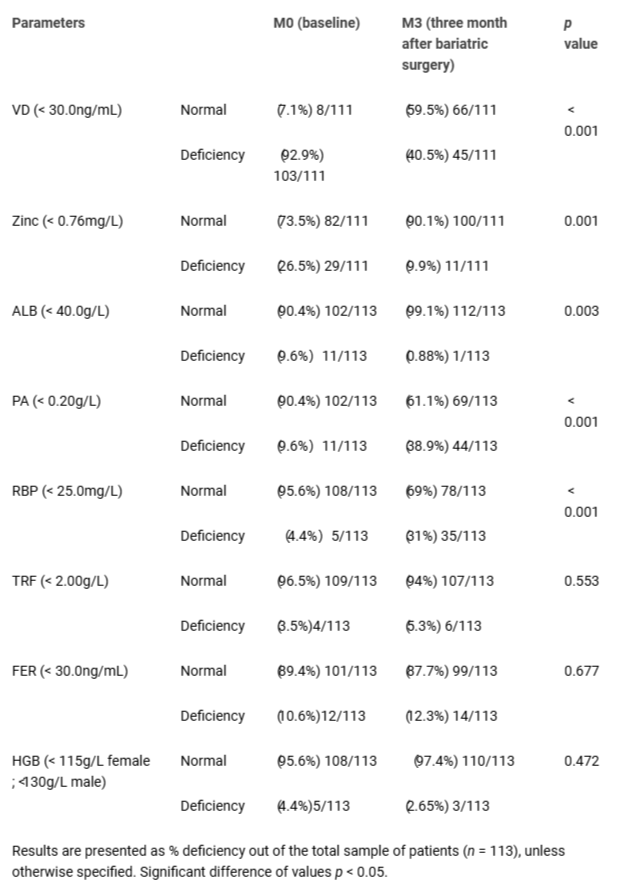 Table 2: Prevalence of nutritional deficiencies at baseline...
Table 2: Prevalence of nutritional deficiencies at baseline...
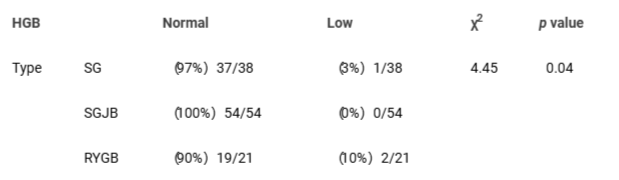 Table 3: Association between postoperative anemia and diffe...
Table 3: Association between postoperative anemia and diffe...
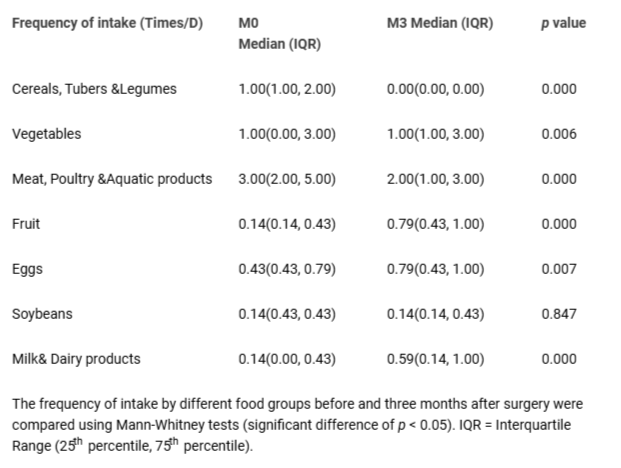 Table 4: Change of intake frequency at baseline (M0) and th...
Table 4: Change of intake frequency at baseline (M0) and th...
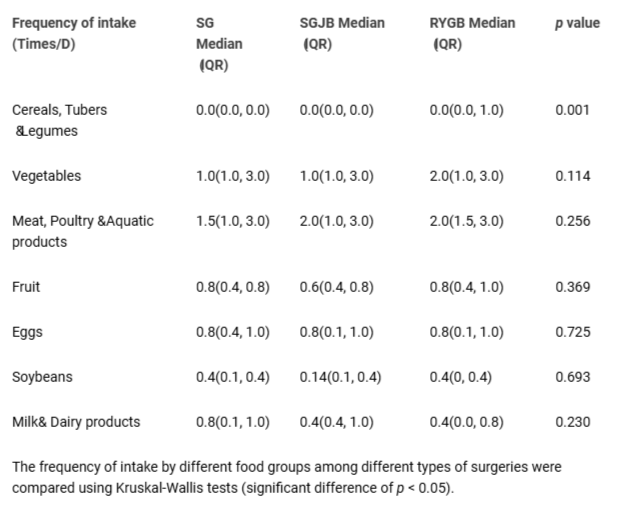 Table 5: Change of intake frequency between different types...
Table 5: Change of intake frequency between different types...
World Health Organization. "WHO Accelerates Work on Nutrition Targets with New commitments 2021[Available from: https://www.who.int/news/item/07-12-2021-who-accelerates-work-on-nutrition-targets-with-new-commitments.
Pan XF, Wang L, Pan A. Epidemiology and determinants of obesity in China. Lancet Diabetes Endocrinol. 2021 Jun;9(6):373-392. doi: 10.1016/S2213-8587(21)00045-0. Erratum in: Lancet Diabetes Endocrinol. 2021 Jul;9(7):e2. doi: 10.1016/S2213-8587(21)00149-2. PMID: 34022156.
GBD 2015 Obesity Collaborators; Afshin A, Forouzanfar MH, Reitsma MB, Sur P, Estep K, Lee A, et al. Health Effects of Overweight and Obesity in 195 Countries over 25 Years. N Engl J Med. 2017 Jul 6;377(1):13-27. doi: 10.1056/NEJMoa1614362. Epub 2017 Jun 12. PMID: 28604169; PMCID: PMC5477817.
Albaugh VL, Kindel TL, Nissen SE, Aminian A. Cardiovascular Risk Reduction Following Metabolic and Bariatric Surgery. Surg Clin North Am. 2021 Apr;101(2):269-294. doi: 10.1016/j.suc.2020.12.012. PMID: 33743969.
Fischer H, Weiss RE, Friedman AN, Imam TH, Coleman KJ. The relationship between kidney function and body mass index before and after bariatric surgery in patients with chronic kidney disease. Surg Obes Relat Dis. 2021 Mar;17(3):508-515. doi: 10.1016/j.soard.2020.11.010. Epub 2020 Nov 19. PMID: 33358080; PMCID: PMC7904605.
Wei Y, Wu T, Tong DKH, Law BTT, Leung DKW, Lam CLK, Wong CKH. Improvement in patient-reported outcomes in Chinese adults after bariatric surgery: 1-year follow-up of a prospective cohort. Surg Obes Relat Dis. 2020 Oct;16(10):1563-1572. doi: 10.1016/j.soard.2020.04.050. Epub 2020 May 15. PMID: 32675022.
The American Society for Metabolic & Bariatric Surgery. 2021 20 April 2022]; Available from: https://asmbs.org/resources/metabolic-and-bariatric-surgery.
Yue TP, Mohd Yusof BN, Nor Hanipah ZB, Gee T. Food tolerance, nutritional status and health-related quality of life of patients with morbid obesity after bariatric surgery. Clin Nutr ESPEN. 2022 Apr;48:321-328. doi: 10.1016/j.clnesp.2022.01.026. Epub 2022 Jan 31. PMID: 35331508.
Mohapatra S, Gangadharan K, Pitchumoni CS. Malnutrition in obesity before and after bariatric surgery. Dis Mon. 2020 Feb;66(2):100866. doi: 10.1016/j.disamonth.2019.06.008. Epub 2019 Jul 10. PMID: 31301800.
Emile, S.H., Elfeki,H, Nutritional Deficiency After Sleeve Gastrectomy: A Comprehensive Literature Review. EMJ Gastroenterol, 2017. 6(1): p. 99-105.
Guan B, Yang J, Chen Y, Yang W, Wang C. Nutritional Deficiencies in Chinese Patients Undergoing Gastric Bypass and Sleeve Gastrectomy: Prevalence and Predictors. Obes Surg. 2018 Sep;28(9):2727-2736. doi: 10.1007/s11695-018-3225-9. PMID: 29754386.
Collazo-Clavell ML, Shah M. Common and Rare Complications of Bariatric Surgery. Endocrinol Metab Clin North Am. 2020 Jun;49(2):329-346. doi: 10.1016/j.ecl.2020.02.003. Epub 2020 Apr 16. PMID: 32418594.
Tan BC, Park YS, Won Y, Lee S, Kang SH, Ahn SH, Park DJ, Kim HH. Preoperative Nutritional Deficiencies in Bariatric Surgery Candidates in Korea. Obes Surg. 2021 Jun;31(6):2660-2668. doi: 10.1007/s11695-021-05318-9. Epub 2021 Mar 8. PMID: 33686579.
Mechanick JI, Apovian C, Brethauer S, Garvey WT, Joffe AM, Kim J, et al. Clinical Practice Guidelines For The Perioperative Nutrition, Metabolic, And Nonsurgical Support Of Patients Undergoing Bariatric Procedures - 2019 Update: Cosponsored By American Association Of Clinical Endocrinologists/American College Of Endocrinology, The Obesity Society, American Society For Metabolic & Bariatric Surgery, Obesity Medicine Association, And American Society Of Anesthesiologists - Executive Summary. Endocr Pract. 2019 Dec;25(12):1346-1359. doi: 10.4158/GL-2019-0406. Epub 2019 Nov 4. PMID: 31682518.
Popkin BM, Du S, Green WD, Beck MA, Algaith T, Herbst CH, Alsukait RF, Alluhidan M, Alazemi N, Shekar M. Individuals with obesity and COVID-19: A global perspective on the epidemiology and biological relationships. Obes Rev. 2020 Nov;21(11):e13128. doi: 10.1111/obr.13128. Epub 2020 Aug 26. Erratum in: Obes Rev. 2021 Oct;22(10):e13305. doi: 10.1111/obr.13305. PMID: 32845580; PMCID: PMC7461480.
Simonnet A, Chetboun M, Poissy J, Raverdy V, Noulette J, Duhamel A, Labreuche J, Mathieu D, Pattou F, Jourdain M; LICORN and the Lille COVID-19 and Obesity study group. High Prevalence of Obesity in Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2) Requiring Invasive Mechanical Ventilation. Obesity (Silver Spring). 2020 Jul;28(7):1195-1199. doi: 10.1002/oby.22831. Epub 2020 Jun 10. Erratum in: Obesity (Silver Spring). 2020 Oct;28(10):1994. doi: 10.1002/oby.23006. PMID: 32271993; PMCID: PMC7262326.
Calder PC. Nutrition, immunity and COVID-19. BMJ Nutr Prev Health. 2020 May 20;3(1):74-92. doi: 10.1136/bmjnph-2020-000085. PMID: 33230497; PMCID: PMC7295866.
Lai NZ, Tan Y, Wang Y. Compositions and methods for treating COVID-19. United States; 2023.
Aron-Wisnewsky J, Verger EO, Bounaix C, Dao MC, Oppert JM, Bouillot JL, Chevallier JM, Clément K. Nutritional and Protein Deficiencies in the Short Term following Both Gastric Bypass and Gastric Banding. PLoS One. 2016 Feb 18;11(2):e0149588. doi: 10.1371/journal.pone.0149588. PMID: 26891123; PMCID: PMC4758752.
Raatz SK, Johnson LK, Caliquary A, King WC, Kalarchian MA, Devlin MJ, Marcus MD, Mitchell JE. Reported nutrient intake over 7 years after Roux-en-Y gastric bypass in the Longitudinal Assessment of Bariatric Surgery-3 (LABS-3) psychosocial study. Surg Obes Relat Dis. 2020 Aug;16(8):1022-1029. doi: 10.1016/j.soard.2020.04.007. Epub 2020 Apr 22. PMID: 32418771; PMCID: PMC7423730.
Calleja-Fernández A, Pintor-de-la-Maza B, Diez-Rodríguez R, Vidal-Casariego A, Urioste-Fondo A, Cano-Rodríguez I, Ballesteros-Pomar MD. Relationship Between Diet and Body Composition After Biliopancreatic Diversion. Obes Surg. 2015 Nov;25(11):2093-9. doi: 10.1007/s11695-015-1658-y. PMID: 26055550.
He Y, Li Y, Yang X, Hemler EC, Fang Y, Zhao L, Zhang J, Yang Z, Wang Z, He L, Sun J, Wang DD, Wang J, Piao J, Liang X, Ding G, Hu FB. The dietary transition and its association with cardiometabolic mortality among Chinese adults, 1982-2012: a cross-sectional population-based study. Lancet Diabetes Endocrinol. 2019 Jul;7(7):540-548. doi: 10.1016/S2213-8587(19)30152-4. Epub 2019 May 10. PMID: 31085143; PMCID: PMC7269053.
Rasaei N, Kashavarz SA, Yekaninejad MS, Mirzaei K. The association between sarcopenic obesity (SO) and major dietary patterns in overweight and obese adult women. Diabetes Metab Syndr. 2019 Jul-Aug;13(4):2519-2524. doi: 10.1016/j.dsx.2019.06.023. Epub 2019 Jul 9. PMID: 31405671.
Roman G, Rusu A, Graur M, Creteanu G, Morosanu M, Radulian G, Amorin P, Timar R, Pircalaboiu L, Bala C. DIETARY PATTERNS AND THEIR ASSOCIATION WITH OBESITY: A CROSS-SECTIONAL STUDY. Acta Endocrinol (Buchar). 2019 Jan-Mar;-5(1):86-95. doi: 10.4183/aeb.2019.86. PMID: 31149065; PMCID: PMC6535323.
Luo JN, Tavakkoli A. Physiologic Mechanisms of Weight Loss Following Metabolic/Bariatric Surgery. Surg Clin North Am. 2021 Apr;101(2):223-237. doi: 10.1016/j.suc.2020.12.006. PMID: 33743966.
Baheeg M, El-Din MT, Labib MF, Elgohary SA, Hasan A. Long-term durability of weight loss after bariatric surgery: a retrospective study. Int J Surg Open. 2021;28:37-40.
Maciejewski ML, Arterburn DE, Van Scoyoc L, Smith VA, Yancy WS Jr, Weidenbacher HJ, Livingston EH, Olsen MK. Bariatric Surgery and Long-term Durability of Weight Loss. JAMA Surg. 2016 Nov 1;151(11):1046-1055. doi: 10.1001/jamasurg.2016.2317. PMID: 27579793; PMCID: PMC5112115.
Xu T, Wang C, Zhang H, Han X, Liu W, Han J, Yu H, Chen J, Zhang P, Di J. Timing of Maximal Weight Reduction Following Bariatric Surgery: A Study in Chinese Patients. Front Endocrinol (Lausanne). 2020 Sep 15;11:615. doi: 10.3389/fendo.2020.00615. PMID: 33042006; PMCID: PMC7522214.
Celik ZM, Islamoglu AH, Sabuncular G, Toprak HS, Gunes FE. Evaluation of malnutrition risk of inpatients in a research and training hospital: A cross-sectional study. Clin Nutr ESPEN. 2021 Feb;41:261-267. doi: 10.1016/j.clnesp.2020.12.002. Epub 2020 Dec 23. PMID: 33487274.
Sensi M, Bruno MR, Valente L, Cioccia GP, Chianelli M, Pozzilli P. Retinol binding protein: a short half life determinant of protein non enzymatic glycation in diabetes. Diabetes Res. 1990 Apr;13(4):195-8. PMID: 2134212.
Li JD, Diao YK, Li J, Wu H, Sun LY, Gu WM, Wang H, Chen TH, Zeng YY, Zhou YH, Wang Y, Zhang YM, Liang YJ, Lau WY, Li C, Liang L, Wang MD, Zhang CW, Shen F, Shao CH, Yang T. Association between preoperative prealbumin level and postoperative mortality and morbidity after hepatic resection for hepatocellular carcinoma: A multicenter study from a HBV-endemic area. Am J Surg. 2021 May;221(5):1024-1032. doi: 10.1016/j.amjsurg.2020.08.036. Epub 2020 Sep 2. PMID: 32951853.
Neyra NR, Hakim RM, Shyr Y, Ikizler TA. Serum transferrin and serum prealbumin are early predictors of serum albumin in chronic hemodialysis patients. J Ren Nutr. 2000 Oct;10(4):184-90. doi: 10.1053/jren.2000.16325. PMID: 11070145.
Gomme PT, McCann KB, Bertolini J. Transferrin: structure, function and potential therapeutic actions. Drug Discov Today. 2005 Feb 15;10(4):267-73. doi: 10.1016/S1359-6446(04)03333-1. PMID: 15708745.
Faria SL, Faria OP, Buffington C, de Almeida Cardeal M, Ito MK. Dietary protein intake and bariatric surgery patients: a review. Obes Surg. 2011 Nov;21(11):1798-805. doi: 10.1007/s11695-011-0441-y. PMID: 21590346.
de la Guía-Galipienso F, Martínez-Ferran M, Vallecillo N, Lavie CJ, Sanchis-Gomar F, Pareja-Galeano H. Vitamin D and cardiovascular health. Clin Nutr. 2021 May;40(5):2946-2957. doi: 10.1016/j.clnu.2020.12.025. Epub 2020 Dec 29. PMID: 33397599; PMCID: PMC7770490.
Krzizek EC, Brix JM, Herz CT, Kopp HP, Schernthaner GH, Schernthaner G, Ludvik B. Prevalence of Micronutrient Deficiency in Patients with Morbid Obesity Before Bariatric Surgery. Obes Surg. 2018 Mar;28(3):643-648. doi: 10.1007/s11695-017-2902-4. PMID: 28849358.
Parrott J, Frank L, Rabena R, Craggs-Dino L, Isom KA, Greiman L. American Society for Metabolic and Bariatric Surgery Integrated Health Nutritional Guidelines for the Surgical Weight Loss Patient 2016 Update: Micronutrients. Surg Obes Relat Dis. 2017 May;13(5):727-741. doi: 10.1016/j.soard.2016.12.018. Epub 2017 Jan 19. PMID: 28392254.
Chakhtoura MT, Nakhoul N, Akl EA, Mantzoros CS, El Hajj Fuleihan GA. Guidelines on vitamin D replacement in bariatric surgery: Identification and systematic appraisal. Metabolism. 2016 Apr;65(4):586-97. doi: 10.1016/j.metabol.2015.12.013. Epub 2016 Jan 4. PMID: 26833101; PMCID: PMC4792722.
Chakhtoura MT, Nakhoul NN, Shawwa K, Mantzoros C, El Hajj Fuleihan GA. Hypovitaminosis D in bariatric surgery: A systematic review of observational studies. Metabolism. 2016 Apr;65(4):574-85. doi: 10.1016/j.metabol.2015.12.004. Epub 2015 Dec 19. PMID: 26805016; PMCID: PMC4792683.
Cronin SJF, Woolf CJ, Weiss G, Penninger JM. The Role of Iron Regulation in Immunometabolism and Immune-Related Disease. Front Mol Biosci. 2019 Nov 22;6:116. doi: 10.3389/fmolb.2019.00116. PMID: 31824960; PMCID: PMC6883604.
Wenger MJ, Rhoten SE, Murray-Kolb LE, Scott SP, Boy E, Gahutu JB, Haas JD. Changes in Iron Status Are Related to Changes in Brain Activity and Behavior in Rwandan Female University Students: Results from a Randomized Controlled Efficacy Trial Involving Iron-Biofortified Beans. J Nutr. 2019 Apr 1;149(4):687-697. doi: 10.1093/jn/nxy265. PMID: 30926992; PMCID: PMC6461719.
Bjørklund G, Peana M, Pivina L, Dosa A, Aaseth J, Semenova Y, Chirumbolo S, Medici S, Dadar M, Costea DO. Iron Deficiency in Obesity and after Bariatric Surgery. Biomolecules. 2021 Apr 21;11(5):613. doi: 10.3390/biom11050613. PMID: 33918997; PMCID: PMC8142987.
Gowanlock Z, Lezhanska A, Conroy M, Crowther M, Tiboni M, Mbuagbaw L, Siegal DM. Iron deficiency following bariatric surgery: a retrospective cohort study. Blood Adv. 2020 Aug 11;4(15):3639-3647. doi: 10.1182/bloodadvances.2020001880. PMID: 32766854; PMCID: PMC7422111.
WHO guideline on use of ferritin concentrations to assess iron status in individuals and populations. 2020; Available from: https://www.who.int/publications/i/item/9789240000124.
C-reactive protein concentrations as a marker of inflammation or infection for interpreting biomarkers of micronutrient status. 2014 20 April 2022]; Available from: https://www.who.int/publications/i/item/WHO-NMH-NHD-EPG-14.7.
Benotti PN, Wood GC, Kaberi-Otarod J, Still CD, Gerhard GS, Bistrian BR. New concepts in the diagnosis and management approach to iron deficiency in candidates for metabolic surgery: should we change our practice? Surg Obes Relat Dis. 2020 Dec;16(12):2074-2081. doi: 10.1016/j.soard.2020.08.018. Epub 2020 Aug 27. PMID: 33011074; PMCID: PMC7704546.
Zhang C, Chen X, Li J, Liu Z, Liu W, Zhang J, Zhou Z. Anaemia and Related Nutritional Deficiencies in Chinese Patients with Obesity, 12 Months Following Laparoscopic Sleeve Gastrectomy. Diabetes Metab Syndr Obes. 2021 Apr 12;14:1575-1587. doi: 10.2147/DMSO.S303320. PMID: 33880047; PMCID: PMC8051959.
Kambe T. Metalation and Maturation of Zinc Ectoenzymes: A Perspective. Biochemistry. 2020 Jan 14;59(1):74-79. doi: 10.1021/acs.biochem.9b00924. Epub 2019 Nov 26. PMID: 31718170.
Gilbert R, Peto T, Lengyel I, Emri E. Zinc Nutrition and Inflammation in the Aging Retina. Mol Nutr Food Res. 2019 Aug;63(15):e1801049. doi: 10.1002/mnfr.201801049. Epub 2019 Jun 27. PMID: 31148351.
Mahawar KK, Bhasker AG, Bindal V, Graham Y, Dudeja U, Lakdawala M, Small PK. Zinc Deficiency after Gastric Bypass for Morbid Obesity: a Systematic Review. Obes Surg. 2017 Feb;27(2):522-529. doi: 10.1007/s11695-016-2474-8. PMID: 27885534.
Osadchuk LV, Danilenko AD, Osadchuk AV. [An influence of zinc on male infertility]. Urologiia. 2021 Nov;(5):84-93. Russian. PMID: 34743439.
Soheilipour F, Ebrahimian M, Pishgahroudsari M, Hajian M, Amirkashani D, Ordooei M, Radgoodarzi M, Eskandari D. The prevalence of zinc deficiency in morbidly obese patients before and after different types of bariatric surgery. BMC Endocr Disord. 2021 May 25;21(1):107. doi: 10.1186/s12902-021-00763-0. PMID: 34030687; PMCID: PMC8147400.
Duncan A, Talwar D, Morrison I. The predictive value of low plasma copper and high plasma zinc in detecting zinc-induced copper deficiency. Ann Clin Biochem. 2016 Sep;53(Pt 5):575-9. doi: 10.1177/0004563215620821. Epub 2015 Nov 19. PMID: 26586851.
Kang S, Seo H, Moon HS, Kwon JH, Park YS, Yun CW. The Role of Zinc in Copper Homeostasis of Aspergillus fumigatus. Int J Mol Sci. 2020 Oct 16;21(20):7665. doi: 10.3390/ijms21207665. PMID: 33081273; PMCID: PMC7593903.
Chinese Nutrition Society, Dietary Guidelines for Chinese Residents(2022). 1st ed. 2022, Beijing, China: People's Medical Publishing House. 303-311.
Han A, Sun T, Ming J, Chai L, Liao X. Are the Chinese Moving toward a Healthy Diet? Evidence from Macro Data from 1961 to 2017. Int J Environ Res Public Health. 2020 Jul 23;17(15):5294. doi: 10.3390/ijerph17155294. PMID: 32717812; PMCID: PMC7432933.
Popkin BM. Synthesis and implications: China's nutrition transition in the context of changes across other low- and middle-income countries. Obes Rev. 2014 Jan;15 Suppl 1(0 1):60-7. doi: 10.1111/obr.12120. PMID: 24341759; PMCID: PMC3869101.
Siddiqui S, Zainal H, Harun SN, Sheikh Ghadzi SM. Dietary assessment of pre-diabetic patients by using food frequency questionnaire. A systematic review of study quality, study outcome, study questionnaire and their relative validity and reliability. Clin Nutr ESPEN. 2019 Feb;29:213-223. doi: 10.1016/j.clnesp.2018.10.002. Epub 2018 Nov 8. PMID: 30661689.
Schafer AL, Weaver CM, Black DM, Wheeler AL, Chang H, Szefc GV, Stewart L, Rogers SJ, Carter JT, Posselt AM, Shoback DM, Sellmeyer DE. Intestinal Calcium Absorption Decreases Dramatically After Gastric Bypass Surgery Despite Optimization of Vitamin D Status. J Bone Miner Res. 2015 Aug;30(8):1377-85. doi: 10.1002/jbmr.2467. Epub 2015 May 21. PMID: 25640580; PMCID: PMC4593653.
Ju L, Yu D, Fang H, Guo Q, Xu X, Li S, Zhao L. [Trends and food sources composition of energy, protein and fat in Chinese residents, 1992-2012]. Wei Sheng Yan Jiu. 2018 Sep;47(5):689-704. Chinese. PMID: 30593290.
Huang L, Wang H, Wang Z, Zhang J, Zhang B, Ding G. Regional Disparities in the Association between Cereal Consumption and Metabolic Syndrome: Results from the China Health and Nutrition Survey. Nutrients. 2019 Apr 1;11(4):764. doi: 10.3390/nu11040764. PMID: 30939825; PMCID: PMC6521195.
Cheng M, Wang H, Wang Z, Du W, Ouyang Y, Zhang B. Relationship between dietary factors and the number of altered metabolic syndrome components in Chinese adults: a cross-sectional study using data from the China Health and Nutrition Survey. BMJ Open. 2017 May 29;7(5):e014911. doi: 10.1136/bmjopen-2016-014911. PMID: 28554922; PMCID: PMC5729973.
Kushner RF, Cummings S, Herron DM. Bariatric surgery: postoperative nutritional management. 2020.
Andromalos L, Crowley N, Brown J, Craggs-Dino L, Handu D, Isom K, Lynch A, DellaValle D. Nutrition Care in Bariatric Surgery: An Academy Evidence Analysis Center Systematic Review. J Acad Nutr Diet. 2019 Apr;119(4):678-686. doi: 10.1016/j.jand.2018.08.002. Epub 2018 Nov 1. PMID: 30391396.
Ledoux S, Flamant M, Calabrese D, Bogard C, Sami O, Coupaye M. What Are the Micronutrient Deficiencies Responsible for the Most Common Nutritional Symptoms After Bariatric Surgery? Obes Surg. 2020 May;30(5):1891-1897. doi: 10.1007/s11695-020-04412-8. PMID: 31960214.
Stocker R, Ceyhan M, Schönenberger KA, Stanga Z, Reber E. Nutrient and fluid requirements in post-bariatric patients performing physical activity: A systematic review. Nutrition. 2022 May;97:111577. doi: 10.1016/j.nut.2021.111577. Epub 2021 Dec 24. PMID: 35248847.
Guillet C, Masgrau A, Mishellany-Dutour A, Blot A, Caille A, Lyon N, Pereira B, Slim K, Robert M, Disse E, Feugier N, Le Ruyet P, Louvet C, Miolanne M, Farigon N, Laville M, Boirie Y. Bariatric surgery affects obesity-related protein requirements. Clin Nutr ESPEN. 2020 Dec;40:392-400. doi: 10.1016/j.clnesp.2020.06.007. Epub 2020 Oct 1. PMID: 33183568.
Hirsch KR, Blue MNM, Trexler ET, Ahuja S, Smith-Ryan AE. Provision of ready-to-drink protein following bariatric surgery: An evaluation of tolerability, body composition, and metabolic rate. Clin Nutr. 2021 Apr;40(4):2319-2327. doi: 10.1016/j.clnu.2020.10.022. Epub 2020 Oct 23. PMID: 33158590.
Barnard J, Snowdon D, Hewitson L. Dietary interventions for weight loss and essential aspects of nutrition post–bariatric surgery. In: Practical Guide to Obesity Medicine. 2018;315-327.
Zurbau A, Au-Yeung F, Blanco Mejia S, Khan TA, Vuksan V, Jovanovski E, Leiter LA, Kendall CWC, Jenkins DJA, Sievenpiper JL. Relation of Different Fruit and Vegetable Sources With Incident Cardiovascular Outcomes: A Systematic Review and Meta-Analysis of Prospective Cohort Studies. J Am Heart Assoc. 2020 Oct 20;9(19):e017728. doi: 10.1161/JAHA.120.017728. Epub 2020 Oct 1. PMID: 33000670; PMCID: PMC7792377.
Wang J, Lin X, Bloomgarden ZT, Ning G. The Jiangnan diet, a healthy diet pattern for Chinese. J Diabetes. 2020 May;12(5):365-371. doi: 10.1111/1753-0407.13015. Epub 2020 Jan 26. PMID: 31846221; PMCID: PMC7216939.
Biobaku F, Ghanim H, Monte SV, Caruana JA, Dandona P. Bariatric Surgery: Remission of Inflammation, Cardiometabolic Benefits, and Common Adverse Effects. J Endocr Soc. 2020 Aug 4;4(9):bvaa049. doi: 10.1210/jendso/bvaa049. PMID: 32775937; PMCID: PMC7402590.
Tan Y, Mo Y, Lai NZ. CCL18 induces healthy fibroblast-like synoviocytes to develop gene expression profiling similar to fibroblast-like synoviocytes of rheumatoid arthritis. Cytokines 2020 Virtual Meeting – Abstract Book. 2020:60-61.
Tan Y, Mo Y, Lai NZ. PITPMN3 is a potential gene therapy target to treat rheumatoid arthritis in fibroblast-like synoviocytes by inhibiting CCL18 associated effect, which might activate Toll-like receptor pathway. Mol Ther. 2021;29(4):368.
Tan Y, Hu N, Wu X. The role of CCL18 in rheumatoid arthritis diseases. IgMin Res. 2025;3(1):021-026.