
A New Modification of Classification of Traumatic Patients with Pelvic Fracture
TraumaReceived 27 Mar 2025 Accepted 14 Apr 2025 Published online 15 Apr 2025
Focusing on Biology, Medicine and Engineering ISSN: 2995-8067 | Quick Google Scholar
Next Full Text
Risks and Effects of Medicinal Plants as an Adjuvant Treatment in Mental Disorders during Pregnancy


Received 27 Mar 2025 Accepted 14 Apr 2025 Published online 15 Apr 2025
Background/Purpose: In recent years, the occurrence of pelvic fractures resulting from high-energy trauma has been steadily rising due to the accelerated advancement of the transportation sector. These types of which are associated with high rates of mortality and disability. This study aims to show essential viewpoints regarding quadrilateral plate fracture and classification.
Method: During the period from September 2022 to December 2023, data collected from two hospitals in Xianning city, China, including patients diagnosed with pelvic fractures. Moreover, the patients were included in the analysis after applying specific inclusion and exclusion criteria. The collected data, including age, gender, mechanism of injury, follow-up time, operation time, associated diseases, and associated fractures, were analyzed using SPSS version 22. Applied a modified classification method, and incorporating details about bilateral fractures, proximal femur fractures, and sacrum abnormalities.
Result: This study included 60 patients with a mean age of 49.5 ± 12.3 years, comprising 32 males and 28 females. The majority of fractures caused by traffic accidents (71.7%), followed by falls (28.3%). The mean follow-up time was 8.9 ± 2.3 months. Diabetes, hypertension, heart failure, and dementia were among the associated diseases, with diabetes being the most common (68.3%). Unilateral abnormalities observed in 63.9% of patients, while bilateral abnormalities were seen in 36.1%.
Conclusion: The APQ-SF classification plays an essential role in treatment planning through assessing the stability of the pelvic fracture, enabling effective anatomical reduction and rigid internal fixation. Moreover, can reduce the need for expensive 3D printing for fracture assessment, making the treatment approach more efficient and cost-effective.
In recent years, with the swift development of the transportation, the frequency of pelvic fractures caused by high-energy trauma has been increasing annually, and are associated with high mortality and disability [,]. Surgical treatment of pelvic and acetabular fractures has always been a challenge in the field of trauma orthopedics. For acetabular fractures, anatomical reduction and rigid internal fixation remain the "gold standard" for treatment [,].
As mentioned earlier, the quadrilateral (QL) surface of the acetabulum, considered the third structural column connecting the anterior and posterior acetabular columns plays a vital role in maintaining even pressure contact between the femoral head and the weight-bearing area of the articular surface [,]. It also provides support to prevent posterior and medial displacement of the femoral head. Therefore, fractures of the QL surface can lead to changes in the corresponding joint relationship, imbalance between the femoral head and the acetabulum, and subsequent overall mechanical acetabulum imbalance. Hence, surgical treatment is often necessary for QL surface fractures. Indirect reduction of the acetabulum can be achieved through reduction of the QL area, restoring the integrity of the QL surface and the acetabulum as a whole, thereby achieving satisfactory clinical outcomes [,].
The concept of the QL surface of the acetabulum, also known as the QL area or tetrahedron, was first introduced by Judet, et al. in 1961 []. It is the four-sided region formed by the convergence of the anterior and posterior columns of the acetabulum on its inner side [,]. The upper boundary of the QL surface is a curved line, whereas the lower is the upper edge of the ischial tuberosity, and the lower part of the vertical body of the ischium. The anterior border is the posterior edge of the obturator foramen, and the posterior border is the greater sciatic notch.
During weight-bearing activities such as walking, it primarily ensures continuity between the femoral head and the weight-bearing area of the acetabulum, ensuring even distribution of pressure on the weight-bearing surface of the acetabulum. It also provides support to prevent posterior and medial displacement of the femoral head. Marvin Tile and colleagues also referred to it as the third column of the acetabulum [,].
Fractures of the QL surface of the acetabulum are often caused by an inward impact of the femoral head. In severe cases, it can result in central dislocation of the femoral head. Due to the limited soft tissue support between the femoral head and the base of the acetabulum, simple traction is insufficient to achieve reduction of an inwardly displaced QL area. In some cases, the violence of the impact can induce impaction of the femoral head, making reduction through traction impossible, and surgical treatment is commonly required [,].
The QL surface fractures alter the corresponding joint relationship and cause mechanical imbalance between pelvic bones. This imbalance affects the overall mechanical stability of the acetabulum. As the QL surface is located on the inner side of the acetabulum, indirect reduction of the acetabulum can be achieved through reduction of the QL area [,]. However, surgical treatment of QL surface fractures has always been one of the most formidable and difficult procedures. This is mainly due to the deep anatomical location of the fracture site, its proximity to numerous important blood vessels, nerves, and pelvic organs, which makes surgical exposure difficult and carries high risks. Additionally, the QL area itself has thin bone quality and is adjacent to the articular acetabulum area, further complicating the surgical procedure with limited operative space. Traditional plates and screws are not ideal for fixation, as they can easily penetrate the joint and cause damage to surrounding vital structures [,,]. This study aimed to propose a significant perspective for enhancing pelvic fracture classification and minimizing the reliance on 3D printing.
During the period September 2022 to Dec 2023, the patients were enrolled from two different hospitals (Second Affiliated Hospital of Hubei University of Science and Technology and Xianning Zhongxin Hospital) in Xianning city, Hubei, China after trauma and diagnosed with pelvic fracture. Moreover, we included all traumatic patients with pelvic fractures, whether or not they were associated with other fractures, provided they had more than 6 months of follow-up. Patients were excluded if they died after admission, had less than 6 months of follow-up, incomplete preoperative imaging, or no QL plate fracture.
This study encompassed 60 patients recruited from two hospitals. The collected data, which included variables such as age, gender, mechanism of injury (MOI), follow-up duration, operation time, co-existing diseases, and associated fractures, were analyzed using IBM SPSS Statistics v22. Descriptive statistics and t-tests were used where appropriate. Moreover, statistical analyses were performed to explore potential associations and differences among these variables, aiming to draw meaningful inferences regarding the research objectives.
We modified the classification of pelvic fracture that include more details about bilateral fracture, proximal femur fracture, and sacrum abnormalities. Anterior column (A), posterior column (P), quadrilateral plate (Q), sacrum abnormalities (S), and femur abnormalities (F) (Table 1). Moreover, classify every part into 0= no fracture, 1= stable fracture, and 2= unstable fracture. While we defined, stable fracture as a linear fracture without any dislocation and the unstable fracture as a fracture with a dislocation or comminuted fracture.
After successful anesthesia, the patient was placed in a supine position, and the lower abdomen and perineum are routinely disinfected and draped. Additionally, make a Stoppa incision two centimeters above the pubic symphysis, about 12 centimeters long. Moreover, cut the skin in turn, subcutaneously and make a longitudinal incision along the linea alba, separate and retract the rectus abdominis muscle. Stretch the extraperitoneal pelvic organs posteriorly and medially, and stretch the lower abdominal wall muscles, femoral nerve, external iliac blood vessels, and iliopsoas muscles anterolaterally. Fully expose the pubic symphysis to the true pelvic edge of the sacroiliac joint, and ligate the pubic bone to Corona Mortis at its anatomical root. After the reduction effect is satisfactory, an auxiliary incision about six centimeters long is made at the left anterior superior iliac spine, the skin and subcutaneous are incised, and the inner plate of the ilium is peeled off to expose the acetabulum and part of the bone forward and downward, and place it in the acetabulum. The side arm is inserted into a pre-bent butterfly-shaped reconstruction locking plate of appropriate length (model specification: SCLP 15 II type left 16 holes, Company: Dabo Medical Technology Co., Ltd.). Place it above the left superior pubic ramus, drill holes, depth measurement, and screw fixation. C-arm fluoroscopy shows that the fracture alignment and plate screw position are in good condition.
Use an electric pulse irrigator Manufacturer: Guangzhou Jialin Medical Supplies Manufacturing Co., Ltd. Company Specification and Model: W-202-C to wash the wound surface and carefully stop bleeding and insert an appropriate amount of allograft bone (deep cancellous bone strip specifications (mm): (20~40)× (mm): (20~40)×(4.5~5.5)×(4.5~5.5) filling volume: three milliliters (the production unit name is Hangzhou Hongli Biomedical Technology Co., Ltd.). packing bone graft, indwelling drainage tube in the wound above the pubic symphysis 1 piece, suture the wound layer by layer, suture the skin with a disposable skin suture device (P-PF-35W), cover it with clean dressing, and add pressure and bandage the incision. The negative pressure suction device of the left calf was removed, the defect wound was draped with routine disinfection, and the wound was repeatedly rinsed with hydrogen peroxide, diluted active iodine saline and normal saline. During the operation, the growth of granulation tissue at the wound was unsatisfactory and no obvious necrotic tissue was found. After subcutaneous separation, make holes and decompress and suture part of the skin to reduce the wound surface, and then use two disposable negative pressure drainage and wound care materials (drainage tube set) (Manufacturer: Wuhan VSD Medical Technology Co., Ltd. specification model: VSD -D-2-15x10x1) covers the wound surface, with normal negative pressure and smooth drainage. In contrast, the intraoperative bleeding was about 300 mL and the patient sent to the ward.
The ethics committee of Hubei University of science and technology, granted approval for this study, No.2024-02-001.
Moreover, this study included 60 patients, the patients’ age range from 23 to 70 years old with a mean age of 49.5 ± 12.3 years old. Moreover, males were 32 (53.3%) and 28 females (46.7%). Regarding the MOI, 43 patients (71.7%) after traffic accident and 17 were after fall (28.3%). Mean follow-up 8.9 ± 2.3 months. Time from trauma to the operation ranged between 12 to 192 hours with a mean 52.1 ± 46.2 hours. However, associated diseases included diabetes, hypertension (HTN), heart failure (HF), and dementia. Whereas diabetes was in 41 patients (67.2%), HTN in 26 patients (42.6%), HF in 7 patients (11.5%), dementia in 2 patients (3.3%), and 19 patients (31.1%) showed clear medical history (Table 2).
According to the preoperative imaging in 60 patients, 39 (63.9%) showed unilateral abnormalities while 21 (36.1%) showed bilateral abnormalities. However, 17 sacroiliac abnormality (fracture or dislocation), 32 femur abnormalities (fracture or dislocation), 6 intertrochanteric fracture, 6 sub-trochanteric fracture, and 6 showed no sacrum or femur abnormalities (Figure 1). However, 10 tibia fracture, 3 L5, 3 fibula fracture, and 4 radius fracture. In these patients, no patient experienced symptoms of obturator nerve palsy after surgery. There were no cases of inguinal hernia, iliac vessel injury, or other complications observed in this group. During the follow-up period and according to the patients history there was no cases of traumatic arthritis or avascular necrosis of the femoral head.
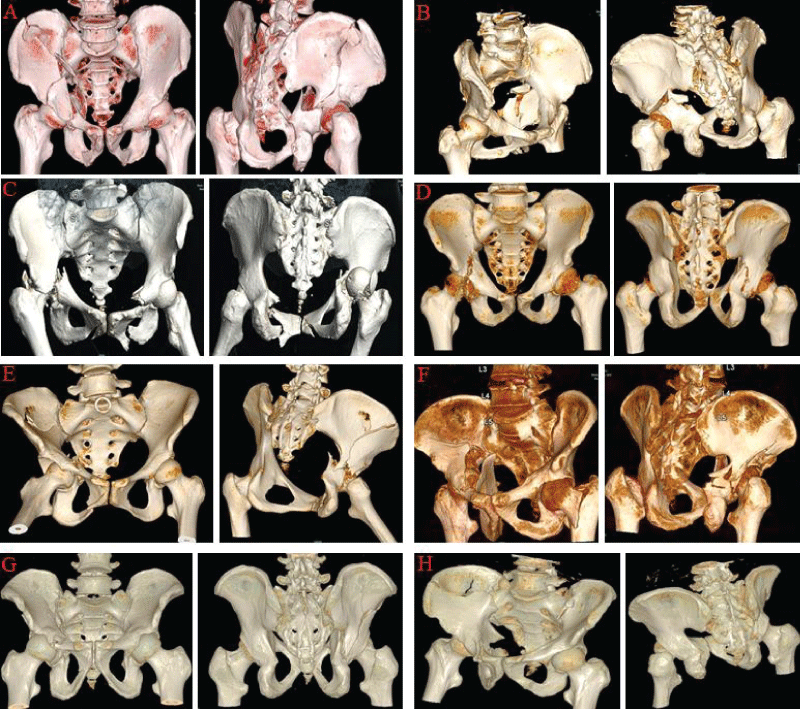 Figure 1: Eight traumatic cases admitted for surgical treatment method and classified as follows: A: 55 years old male after traffic accident (A2, P1, Q2, S0, F0). B: 61 years old female after traffic accident (A1, P2, Q2, S0, F0). C: 63 years old female after traffic accident (A2, P2, Q1, S0, F1). D: 49 years old male after traffic accident (A1,P1,Q1,S0, F1). E: 50 years old female after traffic accident (A1, P2, Q1, S1, F0). F: 37 years old male after fall (A1, P1, Q2, S0, F0). G: 35 years old male after traffic accident (A1, P1, Q1, S0, F0). H: 51 years old male after fall (A1, P1, Q1, S0, F0). F0: No femur fracture; F1: femur has fracture or dislocation; A0: no fracture in anterior column; A1: stable fracture in the anterior column; P0: no fracture in posterior column; P1: fracture in the anterior column; P2: unstable fracture in the posterior column; S0: no abnormality in the sacrum; S1: sacrum is affected; Q0: no fracture in the quadrilateral plate; Q1: stable fracture in the quadrilateral plate; Q2: unstable fracture in the quadrilateral plate.
Figure 1: Eight traumatic cases admitted for surgical treatment method and classified as follows: A: 55 years old male after traffic accident (A2, P1, Q2, S0, F0). B: 61 years old female after traffic accident (A1, P2, Q2, S0, F0). C: 63 years old female after traffic accident (A2, P2, Q1, S0, F1). D: 49 years old male after traffic accident (A1,P1,Q1,S0, F1). E: 50 years old female after traffic accident (A1, P2, Q1, S1, F0). F: 37 years old male after fall (A1, P1, Q2, S0, F0). G: 35 years old male after traffic accident (A1, P1, Q1, S0, F0). H: 51 years old male after fall (A1, P1, Q1, S0, F0). F0: No femur fracture; F1: femur has fracture or dislocation; A0: no fracture in anterior column; A1: stable fracture in the anterior column; P0: no fracture in posterior column; P1: fracture in the anterior column; P2: unstable fracture in the posterior column; S0: no abnormality in the sacrum; S1: sacrum is affected; Q0: no fracture in the quadrilateral plate; Q1: stable fracture in the quadrilateral plate; Q2: unstable fracture in the quadrilateral plate.The anterior acetabulum wall and column have provided reliable solutions for various acetabular fractures in the early stages, which primarily involve the anterior column [,]. However, the traditional ilioinguinal approach can only access the QL area indirectly and does not present direct illustration of the QL area. Therefore, for simple fractures involving the quadrilateral area (which is connected to the column), the QL area can be indirectly reduced by reducing the column. However, when the QL area displaced medially or when comminuted fracture, the reduction becomes challenging. Although some scholars have proposed widening the intermediate window through the ilioinguinal approach to achieve direct illustration of the QL area, the restricted angle and limited operating space make it difficult to place plates and screws on the surface of the QL area, presenting a challenge for fixation in the QL area using the ilioinguinal approach [,,].
In the 1990s, Hirvensalo and Cole introduced a modified Stoppa approach, which was originally used in general surgery for abdominal wall hernia repair, for the surgical treatment of pelvic and acetabular fractures [,]. Compared to the classic ilioinguinal approach, the modified Stoppa approach does not require dissection of the inguinal canal, iliolumbar vessels, or the sciatic nerve, making the surgical procedure simpler. It provides direct visualization of the acetabular dome and the entire QL area, facilitating the placement of plates and screws on the surface of the QL area. When combined with a lateral iliac fossa approach, it allows for exposure of the whole medial region of the hemipelvis, including the sacroiliac joint [].
Based on the above-mentioned APQ-SF classification for pelvic trauma, we have involved the sacrum and femur stability. Firstly, the general principle of fixation is to achieve a stable framework structure of the pelvic although ensuring adequate blocking fixation of the QL area. Specifically, for isolated unstable or stable fractures of the QL area (A0P0Q1/Q2-S0F0), where the anterior and posterior columns of the acetabulum are intact and the framework structure is normal, only blocking fixation of the QL area is required. For single-column fractures combined with stable or unstable QL area fractures (A1P0Q1/2-S0F0, A0P1Q1/2-S0F0), where the framework structure of the acetabulum remains intact, fixation of the single column is performed although simultaneously blocking fixation of the QL area. For double-column fractures combined with stable or unstable QL area fractures (A1P1Q1/Q2-S0F0), the framework structure of the acetabulum is already disrupted, thus frame fixation is necessary. During the restoration of the dissected position of the posterior column, the QL area is also reduced and fixed. However, in cases of complete QL area fractures, where the QL area is completely separated from the posterior column, frame fixation is performed along with blocking fixation of the QL area. However, if the pelvic fracture is accompanied with a sacrum or femur fixation (S1F1), which will require additional intraoperative plan. Combined the sacrum and femur in the pelvic classification is essential to confirm the preoperative and treatment plan. However, it can make it easier for the physician during the follow-up time and less cost for the patients thereby reducing the need for 3D printing. The 3D printing is a high cost for the patients and it can delay the surgical interventions in a stable patients. CT-3D imaging is often sufficient to understand the fracture stability. Involving the femur fracture with pelvic fracture classification might show better understanding for the patients situation at the onset time.
Anatomical reduction and rigid internal fixation remain the recommended surgical standard of complicated acetabular fractures, as they significantly diminish the risk of post-traumatic arthritis, allow for early mobilization, and improve long-term clinical outcomes [,]. Anatomic reduction of the fracture is crucial for restoring the integrity of the articular surface and reconstructing hip joint function. It is one of the prerequisites for evaluating the success of the surgery. However, maintaining the reduction and achieving secure fixation between fracture fragments are equally important, especially for intra-articular fractures []. Sacrum disruption after the onset can easily missed because the fracture severity and other reasons. So, involving the sacrum stability in this classification is required to approve the understanding of pelvic fracture severity and treatment plan.
For complex acetabular fractures, traditional internal fixation methods include dual plates fixation of the anterior and posterior columns, combination of an anterior column plate with an iliac wing plate, or an anterior column plate combined with periacetabular long screws. These methods have drawbacks such as extensive trauma, cumbersome surgical procedures, and especially the placement of periacetabular long screws, which require high surgical skills and involve risks to blood vessels and nerves. Additionally, the irregular anatomical morphology of the pelvic bone surface poses challenges. When using conventional reconstruction plates, repeated plate bending during surgery may prolong the operation time, reduce the strength of the plate, and potentially lead to secondary displacement of the reduced fracture due to inadequate plate contouring. Therefore, the development of ideal specialized internal fixation devices for acetabular fractures is an urgent clinical need [-]. Disruption of the QL area mostly associated with sacrum and femur stability. However, the treatment of pelvic fracture should involve these areas and confirm the stability that can provide better operative plan.
The traditional classification method of pelvic fractures usually does not consider the impact of sacroiliac joint dislocation and femur fracture, but our study included sacroiliac joint dislocation and femur abnormalities in the classification of pelvic fractures. This can provide a more complete assessment of the severity and complexity of pelvic fractures, helping to develop more accurate preoperative treatment plans. However, by identifying a new classification method for pelvic fractures, we may provide more accurate surgical guidance for treating these patients. Based on the characteristics of different classification types, we can more accurately select appropriate surgical techniques and fixation methods to optimize pelvic stability restoration and function. Additionally, this classification may reduce reliance on 3D printing and lower preoperative planning costs. These points will help improve the understanding and treatment of pelvic fractures, providing patients with more personalized, precise and efficient care.
The study's limitations include a small sample size of 60 patients and its single-center setting, which may impact the generalizability of the findings. The retrospective design, reliance on medical records, and short 6-month follow-up period limit the robustness of the findings. Excluding patients with incomplete records or specific fracture types may overlook significant variables. The study lacks a comparison group and comprehensive discussion of treatment outcomes and patient-reported outcomes. The lack of transparency in patient selection and criteria may introduce selection or reporting bias. Future research should address these limitations to validate and improve the proposed classification method for pelvic fractures.
However, future research should explore the long-term effectiveness of treatment modalities and over extended follow-up periods to better understand their durability. Multicenter studies with large sample sizes are needed to validate the findings from this single-center research, minimizing bias and enhancing generalizability. Moreover, investigating the role of CT-3D in predicting treatment response could revolutionize personalized medicine approaches in the field.
The revised Stoppa approach simplifies surgical procedures for pelvic and acetabular fractures by directly visualizing the QL area. The APQ-SF classification considers the stability of the sacrum and femur, offering structured guidance for surgical planning based on severity and complexity of the fracture. Anatomical reduction and rigid internal fixation remain the preferred methods, while specialized fixation devices are necessary for complex fractures. Including sacroiliac joint dislocation and femur abnormalities in the classification enhances treatment planning. CT-3D imaging is generally adequate for evaluating fracture stability, reducing costs and avoiding delays. This classification may enhance personalized and efficient patient care, reducing the reliance on 3D printing.
Informed consent was obtained from all individual participants included in the study
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee (Hubei University of Science and Technology, No. 2024-02-001) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
The authors thank the Orthopedics department for the support.
Gänsslen A, Frink M, Hildebrand F, Krettek C. Both column fractures of the acetabulum: epidemiology, operative management and long-term-results. Acta Chir Orthop Traumatol Cech. 2012;79(2):107-13. PMID: 22538099.
Perkins ZB, Maytham GD, Koers L, Bates P, Brohi K, Tai NR. Impact on outcome of a targeted performance improvement programme in haemodynamically unstable patients with a pelvic fracture. Bone Joint J. 2014 Aug;96-B(8):1090-7. doi: 10.1302/0301-620X.96B8.33383. PMID: 25086126.
Märdian S, Schaser KD, Hinz P, Wittenberg S, Haas NP, Schwabe P. Fixation of acetabular fractures via the ilioinguinal versus pararectus approach: a direct comparison. Bone Joint J. 2015 Sep;97-B(9):1271-8. doi: 10.1302/0301-620X.97B9.35403. PMID: 26330596.
Chen K, Yang F, Yao S, Xiong Z, Sun T, Zhu F, Telemacque D, Drepaul D, Ren Z, Guo X. Application of computer-assisted virtual surgical procedures and three-dimensional printing of patient-specific pre-contoured plates in bicolumnar acetabular fracture fixation. Orthop Traumatol Surg Res. 2019 Sep;105(5):877-884. doi: 10.1016/j.otsr.2019.05.011. Epub 2019 Jul 9. PMID: 31300239.
Johns BP, Balogh ZJ. The horizontal shear fracture of the pelvis. Eur J Trauma Emerg Surg. 2022 Jun;48(3):2265-2273. doi: 10.1007/s00068-021-01764-3. Epub 2021 Aug 2. PMID: 34338821; PMCID: PMC9192401.
Cheng X, Hou F, Pan Y, Yin Y. Current status and advances in the treatment of quadrilateral plate fractures of the acetabulum. J Chin Foreign Med Treat. 2015;34(22):9-10.
Prasartritha T, Chaivanichsiri P. The study of broken quadrilateral surface in fractures of the acetabulum. Int Orthop. 2013 Jun;37(6):1127-34. doi: 10.1007/s00264-013-1845-1. Epub 2013 Apr 24. PMID: 23613172; PMCID: PMC3664151.
Judet R. Fractures of the acetabulum. Classification and surgical approaches for open reduction. J Bone Joint Surg, A. 1961;43:30-59.
Peng Y, Zhang LH, Tang PF. [Progress on treatment and research of quadrilateral plate fractures of acetabular]. Zhongguo Gu Shang. 2015 May;28(5):472-5. Chinese. PMID: 26193732.
Li Ming, Pang Qingjiang, Zheng Qi. Research Progress on Internal Fixation of Quadrilateral Zone Fractures of the Acetabulum. Chinese Journal of Traumatology. 2017;33(5):470-4.
ElNahal WA, Abdel Karim M, Khaled SA, Abdelazeem AH, Abdelazeem H. Quadrilateral plate fractures of the acetabulum: Proposition for a novel classification system. Injury. 2018 Feb;49(2):296-301. doi: 10.1016/j.injury.2017.11.041. Epub 2017 Dec 1. PMID: 29241997.
Meng Y, Wang M, Gao Z. Treatment strategies for quadrilateral plate fractures of the acetabulum. Chin J Physicians. 2013;(2):232-4.
Liu L, Gao H. Research progress on treatment of quadrilateral plate fractures of the acetabulum. J Gannan Med Univ. 2017;37(3):501-4.
Gao J, Liu S, Feng D, Ding Y. Measurement of safe angle and range for placement of acetabular quadrilateral plate screws in quadrilateral plate fractures. J Pract Clin Med. 2019;(3):22-3,
Letournel E. The treatment of acetabular fractures through the ilioinguinal approach. Clin Orthop Relat Res. 1993 Jul;(292):62-76. PMID: 8519138.
Hirvensalo E, Lindahl J, Böstman O. A new approach to the internal fixation of unstable pelvic fractures. Clin Orthop Relat Res. 1993 Dec;(297):28-32. PMID: 8242945.
Cole JD, Bolhofner BR. Acetabular fracture fixation via a modified Stoppa limited intrapelvic approach. Description of operative technique and preliminary treatment results. Clin Orthop Relat Res. 1994 Aug;(305):112-23. PMID: 8050220.
Shazar N, Eshed I, Ackshota N, Hershkovich O, Khazanov A, Herman A. Comparison of acetabular fracture reduction quality by the ilioinguinal or the anterior intrapelvic (modified Rives-Stoppa) surgical approaches. J Orthop Trauma. 2014 Jun;28(6):313-9. doi: 10.1097/01.bot.0000435627.56658.53. PMID: 24100918.
von Rüden C, Wenzel L, Becker J, Thannheimer A, Augat P, Woltmann A, Bühren V, Perl M. The pararectus approach for internal fixation of acetabular fractures involving the anterior column: evaluating the functional outcome. Int Orthop. 2019 Jun;43(6):1487-1493. doi: 10.1007/s00264-018-4148-8. Epub 2018 Sep 14. PMID: 30215099; PMCID: PMC6525136.
Karim MA, Abdelazeem AH, Youness M, El Nahal WA. Fixation of quadrilateral plate fractures of the acetabulum using the buttress screw: A novel technique. Injury. 2017 Aug;48(8):1813-1818. doi: 10.1016/j.injury.2017.05.028. Epub 2017 May 24. PMID: 28602177.
Qureshi AA, Archdeacon MT, Jenkins MA, Infante A, DiPasquale T, Bolhofner BR. Infrapectineal plating for acetabular fractures: a technical adjunct to internal fixation. J Orthop Trauma. 2004 Mar;18(3):175-8. doi: 10.1097/00005131-200403000-00009. PMID: 15091273.
Schäffler A, Freude T, Stuby F, Höntzsch D, Veltkamp J, Stöckle U, König B. Operative Versorgung von Azetabulumfrakturen mit der neuen Azetabulumflügelplatte [Surgical Treatment of Acetabulum Fractures with a New Acetabulum Butterfly Plate]. Z Orthop Unfall. 2016 Oct;154(5):488-492. German. doi: 10.1055/s-0042-106476. Epub 2016 Jul 1. PMID: 27366952.
Xu Y, Lin C, Zhang L, Lin M, Lai J, Cao S, Peng G, Feng K, Yan G, Cai D, Wang G. Anterograde Fixation Module for Posterior Acetabular Column Fracture: Computer-Assisted Determination of Optimal Entry Point, Angle, and Length for Screw Insertion. Med Sci Monit. 2016 Sep 1;22:3106-12. doi: 10.12659/msm.896313. PMID: 27584820; PMCID: PMC5017690.
Zha GC, Sun JY, Dong SJ, Zhang W, Luo ZP. A novel fixation system for acetabular quadrilateral plate fracture: a comparative biomechanical study. Biomed Res Int. 2015;2015:391032. doi: 10.1155/2015/391032. Epub 2015 Jan 31. PMID: 25802849; PMCID: PMC4329861.
Sedghazar Z, Altahla R, Sadeghi S, Karaminasian M, Li W, Jun L, Alshorman J. A New Modification of Classification of Traumatic Patients with Pelvic Fracture. IgMin Res. April 15, 2025; 3(4): 188-194. IgMin ID: igmin297; DOI:10.61927/igmin297; Available at: igmin.link/p297
Anyone you share the following link with will be able to read this content:
1Cardiology Unit, Hospital Pakar Universiti Sains Malaysia, Kota Bharu, Malaysia
2Department of Rehabilitation, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan 430030, Hubei, China
3Nursing, Xianning Maternal and Child Health Hospital, Hubei, Xiang Ning 437100, China
4Clinical Medical College, Hubei University of Science and Technology, Xiang Ning 437100, Hubei, China
Address Correspondence:
Jamal Alshorman, Department of Orthopedics, Second Affiliated Hospital of Hubei University of Science and Technology, Xiang Ning 437100, Hubei, China, Email: [email protected] or [email protected]
How to cite this article:
Sedghazar Z, Altahla R, Sadeghi S, Karaminasian M, Li W, Jun L, Alshorman J. A New Modification of Classification of Traumatic Patients with Pelvic Fracture. IgMin Res. April 15, 2025; 3(4): 188-194. IgMin ID: igmin297; DOI:10.61927/igmin297; Available at: igmin.link/p297
Copyright: © 2025 Sedghazar Z, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
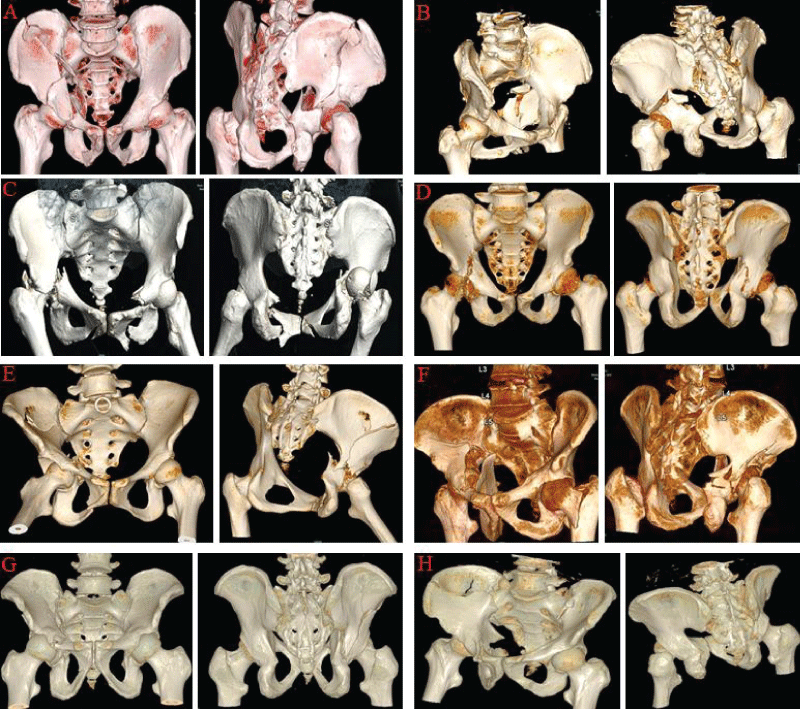 Figure 1: Eight traumatic cases admitted for surgical treatm...
Figure 1: Eight traumatic cases admitted for surgical treatm...
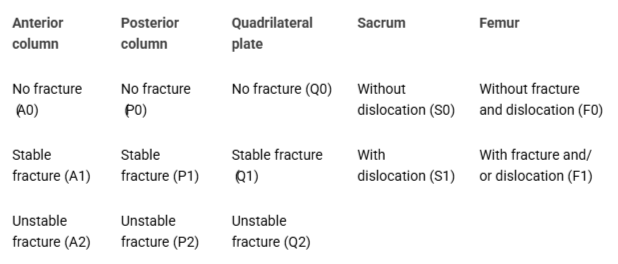 Table 1: Proposed new classification method including the s...
Table 1: Proposed new classification method including the s...
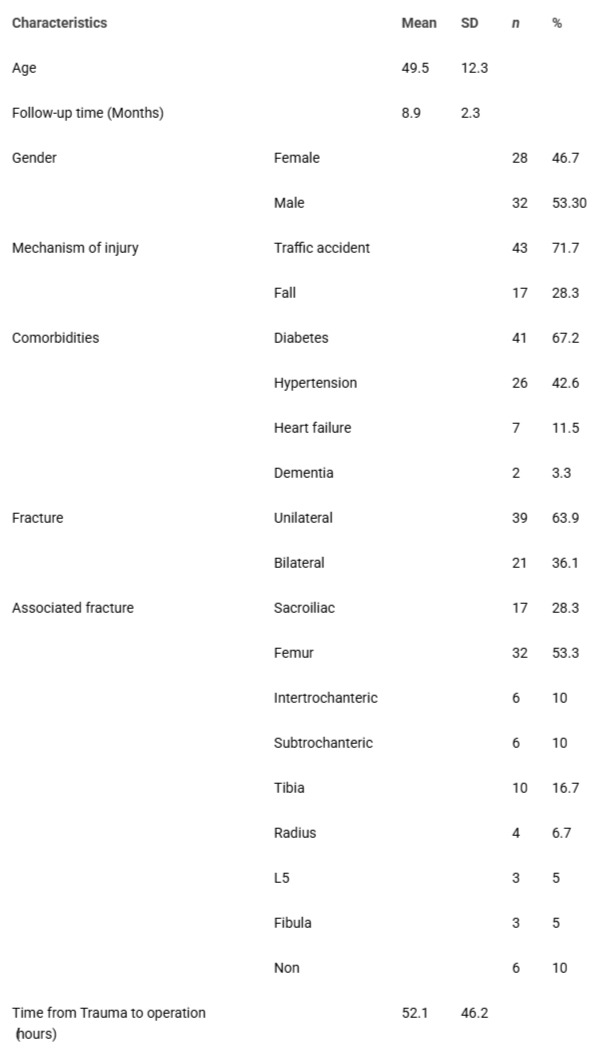 Table 2: Patients summary data....
Table 2: Patients summary data....
Gänsslen A, Frink M, Hildebrand F, Krettek C. Both column fractures of the acetabulum: epidemiology, operative management and long-term-results. Acta Chir Orthop Traumatol Cech. 2012;79(2):107-13. PMID: 22538099.
Perkins ZB, Maytham GD, Koers L, Bates P, Brohi K, Tai NR. Impact on outcome of a targeted performance improvement programme in haemodynamically unstable patients with a pelvic fracture. Bone Joint J. 2014 Aug;96-B(8):1090-7. doi: 10.1302/0301-620X.96B8.33383. PMID: 25086126.
Märdian S, Schaser KD, Hinz P, Wittenberg S, Haas NP, Schwabe P. Fixation of acetabular fractures via the ilioinguinal versus pararectus approach: a direct comparison. Bone Joint J. 2015 Sep;97-B(9):1271-8. doi: 10.1302/0301-620X.97B9.35403. PMID: 26330596.
Chen K, Yang F, Yao S, Xiong Z, Sun T, Zhu F, Telemacque D, Drepaul D, Ren Z, Guo X. Application of computer-assisted virtual surgical procedures and three-dimensional printing of patient-specific pre-contoured plates in bicolumnar acetabular fracture fixation. Orthop Traumatol Surg Res. 2019 Sep;105(5):877-884. doi: 10.1016/j.otsr.2019.05.011. Epub 2019 Jul 9. PMID: 31300239.
Johns BP, Balogh ZJ. The horizontal shear fracture of the pelvis. Eur J Trauma Emerg Surg. 2022 Jun;48(3):2265-2273. doi: 10.1007/s00068-021-01764-3. Epub 2021 Aug 2. PMID: 34338821; PMCID: PMC9192401.
Cheng X, Hou F, Pan Y, Yin Y. Current status and advances in the treatment of quadrilateral plate fractures of the acetabulum. J Chin Foreign Med Treat. 2015;34(22):9-10.
Prasartritha T, Chaivanichsiri P. The study of broken quadrilateral surface in fractures of the acetabulum. Int Orthop. 2013 Jun;37(6):1127-34. doi: 10.1007/s00264-013-1845-1. Epub 2013 Apr 24. PMID: 23613172; PMCID: PMC3664151.
Judet R. Fractures of the acetabulum. Classification and surgical approaches for open reduction. J Bone Joint Surg, A. 1961;43:30-59.
Peng Y, Zhang LH, Tang PF. [Progress on treatment and research of quadrilateral plate fractures of acetabular]. Zhongguo Gu Shang. 2015 May;28(5):472-5. Chinese. PMID: 26193732.
Li Ming, Pang Qingjiang, Zheng Qi. Research Progress on Internal Fixation of Quadrilateral Zone Fractures of the Acetabulum. Chinese Journal of Traumatology. 2017;33(5):470-4.
ElNahal WA, Abdel Karim M, Khaled SA, Abdelazeem AH, Abdelazeem H. Quadrilateral plate fractures of the acetabulum: Proposition for a novel classification system. Injury. 2018 Feb;49(2):296-301. doi: 10.1016/j.injury.2017.11.041. Epub 2017 Dec 1. PMID: 29241997.
Meng Y, Wang M, Gao Z. Treatment strategies for quadrilateral plate fractures of the acetabulum. Chin J Physicians. 2013;(2):232-4.
Liu L, Gao H. Research progress on treatment of quadrilateral plate fractures of the acetabulum. J Gannan Med Univ. 2017;37(3):501-4.
Gao J, Liu S, Feng D, Ding Y. Measurement of safe angle and range for placement of acetabular quadrilateral plate screws in quadrilateral plate fractures. J Pract Clin Med. 2019;(3):22-3,
Letournel E. The treatment of acetabular fractures through the ilioinguinal approach. Clin Orthop Relat Res. 1993 Jul;(292):62-76. PMID: 8519138.
Hirvensalo E, Lindahl J, Böstman O. A new approach to the internal fixation of unstable pelvic fractures. Clin Orthop Relat Res. 1993 Dec;(297):28-32. PMID: 8242945.
Cole JD, Bolhofner BR. Acetabular fracture fixation via a modified Stoppa limited intrapelvic approach. Description of operative technique and preliminary treatment results. Clin Orthop Relat Res. 1994 Aug;(305):112-23. PMID: 8050220.
Shazar N, Eshed I, Ackshota N, Hershkovich O, Khazanov A, Herman A. Comparison of acetabular fracture reduction quality by the ilioinguinal or the anterior intrapelvic (modified Rives-Stoppa) surgical approaches. J Orthop Trauma. 2014 Jun;28(6):313-9. doi: 10.1097/01.bot.0000435627.56658.53. PMID: 24100918.
von Rüden C, Wenzel L, Becker J, Thannheimer A, Augat P, Woltmann A, Bühren V, Perl M. The pararectus approach for internal fixation of acetabular fractures involving the anterior column: evaluating the functional outcome. Int Orthop. 2019 Jun;43(6):1487-1493. doi: 10.1007/s00264-018-4148-8. Epub 2018 Sep 14. PMID: 30215099; PMCID: PMC6525136.
Karim MA, Abdelazeem AH, Youness M, El Nahal WA. Fixation of quadrilateral plate fractures of the acetabulum using the buttress screw: A novel technique. Injury. 2017 Aug;48(8):1813-1818. doi: 10.1016/j.injury.2017.05.028. Epub 2017 May 24. PMID: 28602177.
Qureshi AA, Archdeacon MT, Jenkins MA, Infante A, DiPasquale T, Bolhofner BR. Infrapectineal plating for acetabular fractures: a technical adjunct to internal fixation. J Orthop Trauma. 2004 Mar;18(3):175-8. doi: 10.1097/00005131-200403000-00009. PMID: 15091273.
Schäffler A, Freude T, Stuby F, Höntzsch D, Veltkamp J, Stöckle U, König B. Operative Versorgung von Azetabulumfrakturen mit der neuen Azetabulumflügelplatte [Surgical Treatment of Acetabulum Fractures with a New Acetabulum Butterfly Plate]. Z Orthop Unfall. 2016 Oct;154(5):488-492. German. doi: 10.1055/s-0042-106476. Epub 2016 Jul 1. PMID: 27366952.
Xu Y, Lin C, Zhang L, Lin M, Lai J, Cao S, Peng G, Feng K, Yan G, Cai D, Wang G. Anterograde Fixation Module for Posterior Acetabular Column Fracture: Computer-Assisted Determination of Optimal Entry Point, Angle, and Length for Screw Insertion. Med Sci Monit. 2016 Sep 1;22:3106-12. doi: 10.12659/msm.896313. PMID: 27584820; PMCID: PMC5017690.
Zha GC, Sun JY, Dong SJ, Zhang W, Luo ZP. A novel fixation system for acetabular quadrilateral plate fracture: a comparative biomechanical study. Biomed Res Int. 2015;2015:391032. doi: 10.1155/2015/391032. Epub 2015 Jan 31. PMID: 25802849; PMCID: PMC4329861.